LETTER
Women's Depression: Before Or After Marriage, When Women Are More Depressed?
Sharmin Sultana1, Faisal Muhammad1, *, Alauddin Chowdhury ABM1
Article Information
Identifiers and Pagination:
Year: 2023Volume: 16
E-location ID: e187435012212221
Publisher ID: e187435012212221
DOI: 10.2174/18743501-v16-e230130-2022-47
Article History:
Received Date: 29/4/2022Revision Received Date: 7/9/2022
Acceptance Date: 1/11/20222
Electronic publication date: 01/02/2023
Collection year: 2023

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Dear Editor
Depression is a widespread mental illness. It is distinguished by persistent sadness and a loss of interest or pleasure in previously rewarding or pleasurable activities. It can also interfere with sleep and appetite. Tiredness and lack of concentration are common symptoms [1]. Depression is a chief reason for the Global Burden of Disease [2]. It is estimated that 3.8% population in the world suffers from depression. Around 280 million people worldwide suffer from depression [3]. According to a new study published in The Lancet, the overall number of mental diseases increased considerably in 2020, with an additional 53.2 million cases of depression [4]. Depression has a high lifetime prevalence; associated disability, chronic course, and recurrence have been noted [5]. In addition, depression has a frequent relationship with other prevalent chronic medical illnesses (e.g., diabetes, angina, asthma, arthritis, etc.), and the incremental worsening of their outcomes has been established [5].
There are gender differences in the rates of prevalent mental diseases, especially depression [6]. For example, a recent study shows women suffer from significant depression more often than their male counterparts [7, 8]. Additionally, women are 1.5 to 3 times more likely than men to experience a major depressive episode at some point in their life, with percentages ranging from 6.0 to 17.0 percent [9]. Furthermore, in 2010 the global prevalence of depression among women and men was reported to be 5.5% and 3.2%, respectively, indicating a 1.7-fold increase in women [10, 11].
A study reported that 15.0% of married women were at risk of depression [12]. Also, another study conducted among married women found that 33.3% of participants were depressed [13]. Furthermore, one recent study revealed that 20.1% of married women suffer from severe depression [14]. On the other hand, another study found that depressive symptoms are 17.0% among unmarried women [15]. Depression status is not the same in different stages in women's life. Married women suffer more depression than unmarried ones [16]. A comparative study conducted on 100 working women (an equal number of married and unmarried) concludes that compared to unmarried women, married women have a higher rate of depression [17]. Also, another comparative study conducted on 320 participants, where 160 were married and 160 were unmarried women, revealed that married women were more depressed than unmarried women [18]. On the contrary, according to one study, married women are less likely than unmarried women to report depressive symptoms [19].
There are several reasons behind women's depression. For example, a previous study showed that age, possession of own vehicle, years of schooling, and recent family deaths were significantly associated with depression among married women [13].
Pregnancy is one of the most challenging times in a woman's life, with significant physical, mental, and sexual well-being [20]. Depression associated with childbearing can occur during pregnancy (prenatal depression), after birth (postnatal depression), or both (perinatal depression) [21]. According to several research studies, common mental disorders (depression and anxiety) during pregnancy range from 4.0% to 25.0% [22, 23]. Prevalence rates of prenatal depression during the early weeks of pregnancy were reported to be 5.19% in one study [24]. According to the findings of another study, the rate of prenatal depression was 35.7% [25]. Over one-third of women worldwide experience physical or sexual violence; the lifetime prevalence of violence ranges from 10.0 to 69.0%, with intimate partner violence accounting for most cases [26]. The presence of domestic violence was found to impose a five times higher and highly significant risk of developing prenatal depression among women [27]. Prenatal depression has been linked to occupation, domestic violence, and a lack of social support [27]. The prevalence of postpartum depression was 15.6% to 39.4% [28-30]. Postpartum depression was linked to being widowed/widower, having limited social support, having a present hospitalized child, having experienced the death of a family member or close relative, having an abortion history, having low birth weight, gestational age below 36 weeks, unplanned pregnancy, relatives' mental illness, had no antenatal and postnatal visit [28, 30]. Postpartum depression was linked with job involvement after child delivery, job loss due to pregnancy, history of miscarriage or stillbirth or child death, unintended pregnancy, management of delivery cost by borrowing, selling, or mortgaging assets, depressive symptoms during pregnancy, and intimate partner violence [30]. The prevalence of peripartum depression was 14.0% [31]. Emergency Caesarean sections and unemployment have been linked to the development of peripartum depression [32].
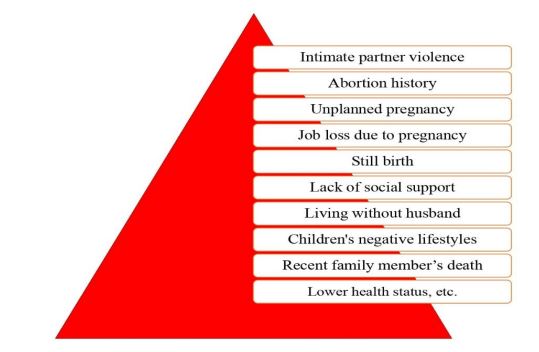 |
Fig (1). Common factors associated with depression among both married and unmarried women at a glance. |
Additionally, mothers of young children are more likely to develop depression and mental health disorders [33]. One recent study revealed that the rate of depression among mothers of young children is so high as well as pointed out the link between children's lifestyles and behavioral factors, such as child's temperament, television watching, and internet use, with the elevated level of depression among mothers [34]. Besides mother's depression is associated with a child's sickness [34]. Furthermore, lower self-rated health status is one of the causes of feelings of depression among unmarried women [35].
Human being likes to see dreams; women want to see visions more. They dream about future life partners, family, and children. Marriage is the beginning of a new chapter in a women's life. Although unmarried women are worried about their poor health status, they get more depressed after marriage. Intimate partner violence, abortion history, unplanned pregnancy, job loss due to pregnancy, stillbirth, lack of social support, living without a husband, children's harmful lifestyles, recent family member's death, etc., are linked with women's depression after marriage (Fig. 1). Women need mental support, especially after marriage. They need help from their family, particularly their husbands. Moreover, the psychological distress, marital dissatisfaction, and general unhappiness of married women were all adversely correlated with husbands' engagement in housework [36]. So, we strongly recommend that the husband always be by his wife's side, give her more time, and take care of her. We suggest that more studies on mental health care for married women should be done in the future.
CONFLICT OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
REFERENCES
| [1] | World Health Organization (WHO). Depression. Available from: https://www.who.int/health-topics/depression#tab=tab_1 [Accessed on August 28, 2022]. |
| [2] | Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med 2013; 10(11): e1001547. |
| [3] | Global Health Data Exchange (GHDx). GBD Results Tool. 2022. Available from: https://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/d780dffbe8a381b25e1416884959e88b [Accessed on August 28, 2022]. |
| [4] | Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021; 398(10312): 1700. |
| [5] | Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007; 370(9590): 851-8. |
| [6] | World Health Organization (WHO). Gender and Mental Health 2022. Available from: https://www.euro.who.int/en/health-topics/health-determinants/gender/activities/gender-and-non-communicable-diseases/gender-and-mental-health [Accessed on April 10, 2022]. |
| [7] | Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry 2000; 57(1): 21-7. |
| [8] | Ford DE, Erlinger TP. Depression and C-reactive protein in US adults. Arch Intern Med 2004; 164(9): 1010-4. |
| [9] | Keyes CL, Goodman SH, Eds. Women and depression: A handbook for the social, behavioral, and biomedical sciences. Cambridge University Press 2006. |
| [10] | Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013; 382(9904): 1575-86. |
| [11] | Baxter AJ, Scott KM, Ferrari AJ, Norman RE, Vos T, Whiteford HA. Challenging the myth of an “epidemic” of common mental disorders: trends in the global prevalence of anxiety and depression between 1990 and 2010. Depress Anxiety 2014; 31(6): 506-16. |
| [12] | Islam MA, Efat SA, Yousuf AB, Islam S. Depression of married women: Exploring the role of employment status, marital satisfaction and psychological well-being. Dhaka Uni J Biol Sci 2016; 25(2): 113-21. |
| [13] | Bhamani SS, Farooq S, Parpio Y, et al. Factors affecting depression among married women living in urban squatter settlements of Karachi, Pakistan. Open J Epidemiol 2016; 6(1): 80-7. |
| [14] | Sultana S, Zaman S, Chowdhury ABMA, et al. Prevalence and factors associated with depression among the mothers of school-going children in Dhaka city, Bangladesh: A multi stage sampling-based study. Heliyon 2021; 7(7): e07493. |
| [15] | Fekih L, Mounis B. The psychological effects of unmarried women “a field study on a sample of unmarried women in Algeria”. Eur Psychiatry 2017; 41(S1): s902. |
| [16] | Wu X, DeMaris A. Gender and marital status differences in depression: The effects of chronic strains. Sex Roles 1996; 34(5-6): 299-319. |
| [17] | Akhouri D, Madiha M, Ansari MH. Anxiety depression and quality of life among working married and unmarried women: a comparative study. Indian J Psychiatr Soc Work 2019; 10(2): 36-9. |
| [18] | Taneja N, Gupta S, Kapoor SK, Kumar A. Comparison of mental health status of married and unmarried girls of late adolescent age in an urban slum of Delhi. Indian J Community Med 2020; 45(2): 145-8. |
| [19] | Earle JR, Smith MH, Harris CT, Longino CF Jr. Women, marital status, and symptoms of depression in a midlife national sample. J Women Aging 1997; 10(1): 41-57. |
| [20] | Senobari M, Azmoude E, Mousavi M. The relationship between body mass index, body image, and sexual function: A survey on Iranian pregnant women. Int J Reprod Biomed (Yazd) 2019; 17(7): 503-12. |
| [21] | Ogbo FA, Eastwood J, Hendry A, et al. Determinants of antenatal depression and postnatal depression in Australia. BMC Psychiatry 2018; 18(1): 49. |
| [22] | Rich-Edwards JW, Kleinman K, Abrams A, et al. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health 2006; 60(3): 221-7. |
| [23] | Pereira PK, Lovisi GM, Pilowsky DL, Lima LA, Legay LF. Depression during pregnancy: prevalence and risk factors among women attending a public health clinic in Rio de Janeiro, Brazil. Cad Saude Publica 2009; 25(12): 2725-36. |
| [24] | Tang X, Lu Z, Hu D, Zhong X. Influencing factors for prenatal Stress, anxiety and depression in early pregnancy among women in Chongqing, China. J Affect Disord 2019; 253: 292-302. |
| [25] | Sheeba B, Nath A, Metgud CS, et al. Prenatal depression and its associated risk factors among pregnant women in Bangalore: a hospital-based prevalence study. Front Public Health 2019; 7: 108. |
| [26] | World Health Organisation (WHO). Global and Regional Estimates of violence against women Available from: http://www.who.int/reproductivehealth/publications/violence/9789241564625/en/ [Accessed on: August 28, 2022]. |
| [27] | Mirieri H. Determinants of prenatal depression among women attending the antenatal clinic at a referral facility in Mombasa County, Kenya: A case control study. Floo Res 2020; 9: 36. |
| [28] | Wubetu AD, Engidaw NA, Gizachew KD. Prevalence of postpartum depression and associated factors among postnatal care attendees in Debre Berhan, Ethiopia, 2018. BMC Pregnancy Childbirth 2020; 20(1): 189. |
| [29] | Azad R, Fahmi R, Shrestha S, et al. Prevalence and risk factors of postpartum depression within one year after birth in urban slums of Dhaka, Bangladesh. PLoS One 2019; 14(5): e0215735. |
| [30] | Asaye MM, Muche HA, Zelalem ED. Prevalence and predictors of postpartum depression: Northwest Ethiopia. Psychiatry J 2020; 2020: 1-9. |
| [31] | Sidhu T, Sidhu G, Kaur P, Lal D, Sangha N. Evaluation of peripartum depression in females. Int J Appl Basic Med Res 2019; 9(4): 201-5. |
| [32] | Duma N, Madiba T. The prevalence of peripartum depression and its relationship to mode of delivery and other factors among mothers in Ixopo, Kwazulu-Natal, South Africa. S Afr J Psychol 2020; 50(4): 530-9. |
| [33] | Surkan PJ, Ettinger AK, Ahmed S, Minkovitz CS, Strobino D. Impact of maternal depressive symptoms on growth of preschool- and school-aged children. Pediatrics 2012; 130(4): e847-55. |
| [34] | Sultana S, Muhammad F, Chowdhury AA, Mistry SK. Child-related factors associated with depressive symptoms among mothers in urban Bangladesh: A Cross-Sectional Study |
| [35] | Mayo Clinic. Rural, Unmarried Women At Higher Risk For Depression, Study Suggests. 2008. Available from: https://www.sciencedaily.com/releases/2008/06/080611154211.htm [Access on April 10, 2022]. |
| [36] | Khawaja M, Habib RR. Husbands’ involvement in housework and women’s psychosocial health: findings from a population-based study in Lebanon. Am J Public Health 2007; 97(5): 860-6. |