All published articles of this journal are available on ScienceDirect.
Traumatic Stress, Psychological Well-being, and Sociodemographic Correlates in High-stress Environments among Healthcare Professionals
Abstract
Background
Healthcare staff provide crucial services to their patients; hence, their well-being is essential to ensure they offer the best services with minimal harm to their health.
Aim
This study aimed to identify associations of traumatic stress, psychological well-being, and sociodemographic variables to provide insight into the experiences and feelings of healthcare personnel in high-stress settings. Furthermore, we will examine how sociodemographic factors and traumatic stress impact the psychological well-being of high-stress environment healthcare professionals.
Objective
This research investigated the relationship between traumatic stress, psychological well-being, and sociodemographic factors in high-stress environments among healthcare personnel in different medical units. It was hypothesized that sociodemographic variables and traumatic stress will predict psychological well-being among healthcare workers who work in high-stress environments. Furthermore, there will be differences in traumatic stress and psychological well-being based on sociodemographic variables among healthcare workers working in high-stress environments.
Methods
To accomplish this goal, an online survey including sociodemographic information, standardized questionnaires of Secondary Traumatic Stress Scale, and a Brief Inventory of Thriving were administered to healthcare personnel (N=290) to collect data for sociodemographic characteristics, traumatic stress levels, and psychological well-being. The results were processed by using SPSS. The descriptive statistics measured participants' characteristics, traumatic stress levels, and psychological well-being. The pearson product-moment correlation, regression analysis, and ANOVA were used to measure the relationship and impact of sociodemographic factors, traumatic stress, and psychological well-being.
Results
A significant inverse relationship between traumatic stress and psychological well-being (r= -0.518, p < 0.05) was reported. Furthermore, multiple regression analysis provided the predictive association of traumatic stress and negative well-being (p<0.05). Additionally, ANOVA was conducted to measure the differences in socio- demographic variables of traumatic stress and the psychological well-being level of healthcare professionals.
Conclusion
The results of this research could help inform policy decisions and interventions that may improve the psychological well-being of healthcare personnel in high-stress environments. Ethical considerations such as participant privacy protection and addressing potential psychological distress are also discussed.
1. INTRODUCTION
Healthcare providers are essential to society because of their impact on people's health and quality of life. The effects of traumatic stress on healthcare professionals can have significant implications for the quality of patient care. Therefore, this study is an effort to explore the association of traumatic stress, psychological well-being (PWB), and sociodemographic characteristics among healthcare professionals working in high-stress conditions across several hospital departments related to emergency, ambulance, and intensive care. According to a systematic review and meta-analysis conducted in twenty-one countries, studies represent a high percentage of depression (21.7%), anxiety (22.1%), and post-traumatic stress disorder (PTSD) (21.5%) among healthcare pro- fessionals during the COVID-19 pandemic [1]. Some other studies confirmed the psychological distress and traumatic stress among HCWs [2, 3]. This high prevalence of mental disorders among healthcare professionals may affect their PWB.
Traumatic stress is a well-established theoretical concept in the field of the psychosocial model, which refers to the psychological response to a traumatic event that is perceived as life-threatening or poses a serious threat to one's physical or psychological integrity [4]. Experiencing traumatic stress has been associated with various unfavorable consequences, such as depression, anxiety, and post-traumatic stress disorder (PTSD). The variable of traumatic stress is drawn from Philip and Cherian's psychosocial stress model [5]. This model suggests that stress arises when people perceive a discrepancy between their goals and the resources available to achieve them. Therefore, healthcare workers (HCWs) can face stress if there is a discrepancy in providing optimal care and available resources. Simultaneously, psychosocial models facilitate under- standing the impact of stressful situations on people. Traumatic stress has been studied as an antecedent or outcome variable. Furthermore, as a predictor variable, exposure to traumatic events may affect an individual's mental health or other outcomes of interest [6]. In addition, studies suggest that people who have been through traumatic experiences are more likely to have concerns with their physical health, such as hypertension, and engage in risky behaviors, such as substance addiction [7]. Traumatic stress may also be seen as an outcome variable, reflecting how traumatic experiences have altered a person's life [8].
Healthcare professionals are often exposed to traumatic events, such as dealing with critically ill patients, experiencing patient deaths, or working in high-stress environments like emergency departments. Traumatic stress may have severe consequences for those working in the medical field, including but not limited to burnout, emotional weariness, depression, anxiety, and PTSD. A study of the relationship between secondary traumatic stress (STS) and occupation found that 53.8% of paramedics, 62.5% of health officers, 67.7% of physicians, 59.3% of emergency medical technicians, 30% of nurses, and 80% of anesthesiologists were affected by trauma experienced by the person being treated or cared for [9]. A cross-sectional study conducted in 2019 among HCWs in Jeddah, Saudi Arabia, found a high prevalence of psychological distress among healthcare workers, with 45.2% of the respondents reporting symptoms of anxiety and 47.6% reporting symptoms of depression [10]. These consequences may affect patient outcomes, work satis- faction, professional progression chances, and general well-being.
On the other hand, PWB is a concept that has received increasing attention in positive psychology research. It is optimal functioning, including positive emotions, engagement, meaning, positive relationships, and accom- plishment [11]. PWB has been linked to various positive outcomes, including better physical health, higher job satisfaction, and greater resilience to stress. Trudel-Fitzgerald et al. [12] describe PWB as a multifaceted construct encompassing objective and subjective elements that incorporate external and tangible factors and internal and subjective experiences. Therefore, the absence of psychological distress and traumatic stress signifies PWB. Traumatic stress and other sociodemographic factors can lead to deteriorated PWB [13]. While PWB is not only an issue of discussion among healthcare professionals in Saudi Arabia [14]. Different factors expose HCW to traumatic stress alongside sociodemographic factors. According to Franzen et al. [15], psychological distress mainly affects psychological well-being.
In this study, we aim to explore how traumatic stress, PWB, and sociodemographic factors interact among healthcare workers (HCWs) in high-stress environments. Specifically, we will examine how sociodemographic factors and traumatic stress predict PWB. By doing so, we hope to better understand the factors that contribute to the PWB of HCWs in high-stress environments and identify potential interventions that can improve their mental health and well-being.
Finally, the relevance of sociodemographic factors is based on the biopsychosocial model, which suggests that social and economic factors strongly influence health outcomes and PWB. For instance, research has indicated that these factors play a role in determining an individual's PWB [16]. Sociodemographic factors such as age, gender, education, and income have been shown to influence both traumatic stress and PWB among HCWs [17]. Some researchers found that nurses in intensive care units in Saudi Arabia experience high-stress levels and tend to be less healthy and less productive [18]. In addition, studies suggest that older individuals, females, and those with lower socioeconomic status may be more likely to experience poorer PWB [19]. According to Philip [5], age plays a significant role in how HCWs evaluate their mental health and PWB. Shamsan and colleagues investigated the occurrence of depression and stress among HCWs in Saudi Arabia [20]. The study revealed that senior HCWs have a significantly increased risk of experiencing isolation, loneliness, despair, and burnout symptoms.
All the existing literature differs from the context of the current investigation. Some studies evaluate only two variables: burnout and PWB or traumatic stress and PWB. A research question has been formulated, ‘Is there a relationship between traumatic stress, psychological well-being, and sociodemographics in high-stress environments among healthcare in different medical units?’ After reviewing the literature, this study proposed the hypothesis, “Sociodemographic variables and traumatic stress will predict psychological well-being among health- care workers who work in high-stress environments.” Furthermore, it is expected that the findings from this research will reveal a difference in responses based on sociodemographic factors, “There will be a difference in responses based on age, gender, experience, education level, or other demographic characteristics when it comes to experiencing traumatic stress and psychological well-being among HCWs.”
2. MATERIALS AND METHODS
2.1. Research Design
This correlational study used quantitative data to determine the effect of traumatic stress, PWB, and sociodemographic factors among healthcare personnel, including trainers, health professionals, and nurses, who were working in emergency, ambulance, and intensive care departments in government hospitals in Saudi Arabia between March 2023 and August 2023. These hospitals are situated in various regions across Saudi Arabia.
2.2. Participants
This study included Saudi and non-Saudi male and female HCWs in government hospitals in Saudi Arabia [21]. The study sample size was selected from 300,000 healthcare personnel in Saudi Arabia. Sampling was gathered from different geographical areas in Saudi Arabia. The sample size was calculated by OpenEpi sampling calculator [22] by using the formula [DEFF*Np(1-p)]/ [(d2/Z21-α/2*(N-1)+p*(1-p)]. Among the participants, 384 HCWs had a hypothesized 50% population, a confidence level of 95%, and a margin of error value = +-5. A total of 384 HCWs were invited to participate in the study, and (290) submitted the complete online survey. Thus, the return rate of the survey was 75%.
2.2.1. Inclusion/ Exclusion Criteria
The study selection was based on the following inclusion criteria: (1) This study's sample of healthcare personnel were trainers, healthcare professionals, and nurses in Saudi Arabia working in emergency, ambulance, and intensive care units.
(2) The personnel in the online survey were between 20 and 65 years old. (3) Before participating in the study, all participants must provide written consent after being informed about the study. However, the exclusion criteria were: (1) Those under 18 years old and those not employed by a medical unit in Saudi Arabia. (2) Participants who do not provide written informed consent will not be in the study.
2.3. Measures
The online survey questionnaires were used in this study. It covered various topics related to traumatic stress, PWB, and sociodemographic factors. Question- naires include questions on participants’ experience with traumatic events, their psychological responses, and demographic characteristics such as gender, age, experience, and educational level.
2.3.1. Sociodemographic Information Form
The Sociodemographic sheet includes the data related to the participants, such as their gender, age, experience, and educational level. The researcher prepared this sociodemographic sheet.
2.3.2. Secondary Traumatic Stress Scale (STSS)
This study used the English version of STSS developed by Bride [23]. This scale has been found to have good validity and reliability in measuring the effects of exposure to traumatic events on medical and mental health personnel. The scale's validity has been established through its ability to differentiate between individuals who have experienced trauma and those who have not [23]. Additionally, the subscales of intrusion, avoidance, and arousal are highly correlated with other measures of trauma- related symptoms, providing further evidence of the scale's validity [23, 24].
STSS is a self-report questionnaire widely used to measure the effects of exposure to traumatic events on medical and mental health personnel. This scale consists of 17 items that measure the levels of STS experienced within the past seven days using a Likert scale ranging from 1 (stating strongly disagree) to 5 (strongly agree). The 17 items were aimed to measure three subscales: i.e., intrusion, avoidance, and arousal [23].
Furthermore, to determine the level of secondary traumatic stress (STS), the scores of each item were added, resulting in a total score, wherein a higher score indicates a more significant occurrence of symptoms. If the score was below 28, the person had little or no STS. A score between 28 and 37 meant the person had mild STS, and between 38 and 43 meant moderate STS, between 44 and 48, meant high STS, and a score of 49 or more meant severe STS. The scores for intrusion, avoidance, and arousal were also calculated by adding specific items. The intrusion score was derived from items 2, 3, 6, 10, and 13, while the avoidance score was derived from items 1, 5, 7, 9, 12, 14, and 17. Finally, the arousal score was derived from items 4, 8, 11,15, and 16.
2.3.3. Brief Inventories of Thriving (BIT)
PWB was measured by the scale Brief Inventories of Thriving (BIT) [25]. It assesses different aspects of psychological health, such as relationships and mastery, and can be completed in just ten items. Participants rate their responses on a scale of 1 to 5, with options ranging from strongly disagree to strongly agree. The scores range from 10 to 50, with varying categories of very low, low, average, high, and very high. The BIT scale has been found to have good validity and reliability in measuring psychological well-being [25]. The scale is positively correlated with other measures of personality and well-being [26]. The scale's internal consistency has been found to be high, with Cronbach's alpha coefficients ranging from .76 to .89 [26]. The test-retest reliability of the scale has also been found to be strong, with correlations ranging from .68 to .80 throughout one to four weeks [26].
2.4. Procedure
The procedure for this study consisted of five steps. Based on the procedure, in the first step of the research, emails were sent to the authors of the scales used in the study to seek permission to use them. In the second step, emails were sent to various Saudi Arabian government hospitals to obtain employee data and understand the target population. Approval from the institutional review board (IRB) was obtained in the third step before requesting government hospitals to partake in the survey in the fourth step. Online consent forms were provided along with detailed information about the research project. Finally, healthcare personnel from different medical units participated in a structured online survey to evaluate the relationship between traumatic stress, PWB, and sociodemographic factors. According to the instructions, participants must fill out the online consent form, and they may leave the survey at any time before completing it. Furthermore, there is no cost to the participant. The survey was online; there was no limited time to fill it out, and the participants could take a break at any time they wanted.
2.5. Ethical Considerations
The approval from the Institutional Review Board at Princess Noura bint Abdulrahman University (Log no. 23-0263) was obtained, and the exemption status was received. In addition, the researcher obtained permission from the authors to use the STS scale. The other scale of BIT was found to be publicly available for research. The primary moral concern for this study was the protection of participants' privacy and confidentiality. Therefore, a consent form was attached to the survey. All survey responses were kept confidential, and any identifying information was converted into codes. In addition, all participants were fully conversant about their rights as subjects and provided an opt-out option. Finally, all data obtained from this study were securely stored, and access to the data was strictly limited. Only researchers involved in the study have access to the data. All measures outlined above ensured that participant privacy was protected and research protocols were adhered to.
2.6. Data Analysis
The results from the survey were analyzed using quantitative methods such as descriptive statistics, including mean, standard deviation, frequencies, and percentages. Moreover, to measure the relation of traumatic stress, PWB, and sociodemographic factors. The person product moment was conducted after checking the normal distribution of scores. These methods were used to measure traumatic stress and PWB and proceeded toward multiple regression and ANOVA. The SPSS version 29 was used with a significance level of p < 0.05.
3. RESULTS
This section describes the various sociodemographic characteristics of study subjects, their psychological well-being and traumatic stress levels, and their interaction and differences according to sociodemographic factors. The alpha coefficient of STS and BIT scales were found as α= 0.843 and α = 0.842 for healthcare professionals in Saudi Arabia.
3.1. Demographic and General Information
The study included 290 participants, with a slightly increased proportion of female representation, with 160 (55.2%) participants. The composition of study subjects was mainly of younger population as those aged 20-29 and 30-39 years represented 43.1% and 34.5% of the study participants, respectively. Moreover, the most significant % of participants (60.7%) had a bachelor’s degree or educational qualification or were doing their internship. Regarding work-related information of the study participants, 39% were health professionals, and more than one-third (39.3%) of the study subjects reported having 1-4 years of experience. Participants working in the emergency, inpatient, and outpatient departments constituted nearly half of the study subjects jointly, representing 25.1% and 22.6%, respectively. Moreover, approximately the proportions of the study subjects were working in the central, western, and eastern regions of Saudi Arabia, with 33.8%, 35.5%, and 27.9%, respectively (Table 1).
| Variables | Categories | f | Percentage |
|---|---|---|---|
| Age in years | 20-29 | 125 | 43.1% |
| 30-39 | 100 | 34.5% | |
| 40-49 | 40 | 13.8% | |
| 50-59 | 23 | 7.9% | |
| 60 or more | 2 | 0.7% | |
| Gender | Female | 160 | 55.2% |
| Male | 130 | 44.8% | |
| Occupation | Health professional | 113 | 39.0% |
| Nursing | 89 | 30.7% | |
| Trainee | 81 | 27.9% | |
| Others | 7 | 2.4% | |
| Educational Qualification | High school/Diploma | 50 | 17.2% |
| Bachelor's degree/ Internship | 176 | 60.7% | |
| Master's degree/ Residency | 37 | 12.8% | |
| Doctorate degree/ Fellowship | 27 | 9.3% | |
| Years of work in specialization | 1-4 | 114 | 39.3% |
| 5-8 | 69 | 23.8% | |
| 9-12 | 55 | 19.0% | |
| 13 or more | 52 | 17.9% | |
| What is your working unit? | Ambulance | 42 | 14.8% |
| Emergency department | 71 | 25.1% | |
| Surgery | 8 | 2.8% | |
| Inpatient and outpatient unit | 64 | 22.6% | |
| Intensive care unit | 47 | 16.6% | |
| Palliative care | 8 | 2.8% | |
| Rotating trainee | 34 | 12.0% | |
| Others | 9 | 3.2% | |
| In which region of KSA are you working? | Central Region | 98 | 33.8% |
| Western Region | 103 | 35.5% | |
| Eastern Region | 81 | 27.9% | |
| Northern Region | 5 | 1.7% | |
| Southern Region | 3 | 1.0% |
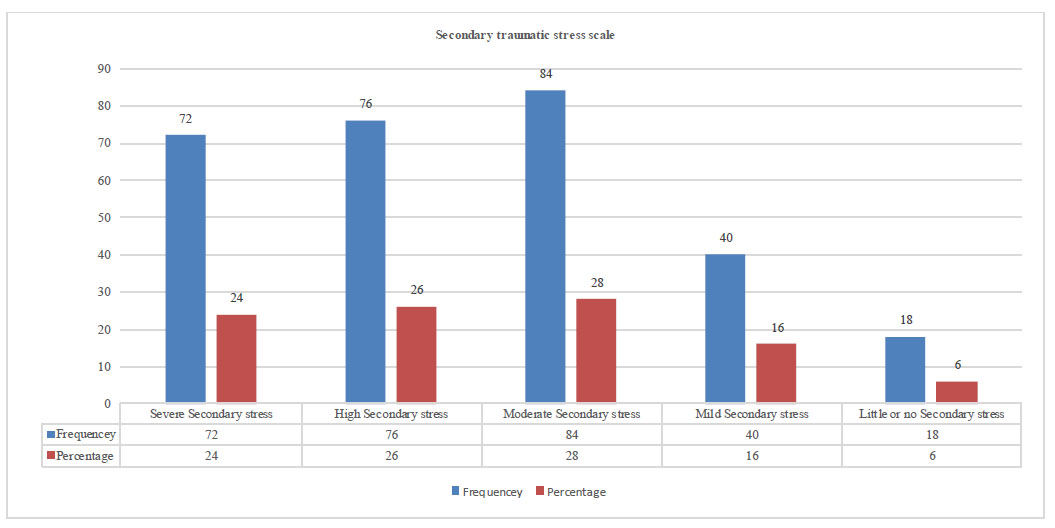
Stress level of participants according to the secondary traumatic stress scale.
Table 2.
| Sub-scales of STS | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Intrusion subscale | 11.1 | 2.8 | 5.0 | 24.0 |
| Avoidance subscale | 17.9 | 2.1 | 7.0 | 31.0 |
| Arousal subscale | 14.0 | 2.3 | 5.0 | 23.0 |
| Secondary traumatic stress scale | 42.9 | 2.9 | 17.0 | 70.0 |
| BIT scale Total Score | 35.5 | 2.4 | 13.0 | 50.0 |
3.2. Secondary Traumatic Stress
The mean (SD) BIT score was 35.5 (2.4), ranging from 13 to 50, while the mean (SD) of the secondary traumatic scale among participants was 42.9 (2.9), ranging from 17 to 70, with means (SD) of 11.1 (2.8), 17.9 (2.1), and 14 (2.3) for the intrusion, avoidance, and arousal subscales, respectively (Table 2), when categorizing secondary traumatic stress levels, about one-quarter (24%) of the participants were found to have severe stress. In comparison, 26%, 28%, and 16% suffered from high, moderate, and mild stress, respectively (Fig. 1).
3.3. Predicting Parameters of Psychological Well-being
An inverse relationship was found between PWB and STS (r= -0.518, p< 0.001). On sociodemographic variables, the female gender was found to be correlated with stress (r= -.161, p<.006), and less experienced professionals in specialization were found to have higher stress levels (r=-.124, p<.034) (Table 3).
Further, analysis of the predicting factors of psychological well-being measured by the BIT scale indicated that secondary traumatic stress was the only factor that significantly negatively affected psychological well-being (B= -2.406, p < .001). None of the socio- demographic factors were statistically significant (Table 4).
3.4. Analysis of Variance
Using the Shapiro-Wilk test, the data were found to be normally distributed for BIT and STSS scales. However, from sociodemographic factors, gender, occupation, working unit, and region were found to be normally distributed. There were significant differences in STS and BIT scores according to gender (p = 0.006 and 0.035), occupation (p = 0.043 and 0.01), and working unit (p= 0.002 and < 0.001). There was also a significant difference according to region of work (p = 0.006), in STSS scores, with the central region having the highest STSS score and the northern region having the lowest. (Table 5).
| Variables | Age | Gender | Educational Qualification | Years of Work in Specialization | Secondary Traumatic Stress Scale |
|---|---|---|---|---|---|
| Gender | .321** | - | - | - | - |
| Educational qualification | .431** | .074 | - | - | - |
| Years of work in specialization | .840** | .355** | .335** | - | - |
| Secondary traumatic stress scale | -.096 | -.161** | .038 | -.124* | - |
| Psychological wellbeing scale (BIT) | .078 | .026 | .034 | .048 | -.518** |
*. Correlation is significant at the 0.05 level (2-tailed).
| Model | Unstandardized Coefficients | Std. Coefficients | t | Sig. | |
|---|---|---|---|---|---|
| B | Std. Error | Beta | |||
| (Constant) | 43.352 | 1.169 | - | 37.088 | .000 |
| Age in years | .551 | .542 | .099 | 1.017 | .310 |
| Gender | -.411 | .587 | -.038 | -.699 | .485 |
| Educational Qualification | .375 | .375 | .056 | .998 | .319 |
| Years of work in specialization | -.600 | .450 | -.125 | -1.332 | .184 |
| Secondary traumatic stress | -2.406 | .230 | -.537 | -10.470 | .000 |
Table 5.
| Variables |
Secondary Traumatic stress Scale |
BIT Scale | |||
|---|---|---|---|---|---|
| M (SD) |
Corrected P |
M(SD) |
Corrected P |
||
| Gender | Female | 44.3 (2.9) | 0.000 | 35.3 (1.7) | 0.002 |
| Male | 41.3 (2.3) | 35.6 (1.8) | |||
| Occupation | Health professional | 41.2 (2.3) | 0.002 | 36.4 (1.9) | 0.006 |
| Nursing | 43.9 (2.4) | 35.6 (1.5) | |||
| Trainee | 43.8 (2.1) | 34.4 (1.6) | |||
| Others | 48.4 (2.5) | 31.1 (0.2) | |||
| What is your working unit? | Ambulance | 46.2 (0.3) | 0.0002 | 32.9 (3.1) | 0.000 |
| Emergency department | 44.9 (0.23) | 34.5 (1.6) | |||
| Surgery | 44.1 (1.2) | 39.6 (1.9) | |||
| Inpatient and outpatient unit | 42.1 (1.12) | 36.3 (1.8) | |||
| Intensive care unit | 40.0 (0.8) | 37.6 (2.1) | |||
| Palliative care | 38.3 (1.0) | 40.9 (2.3) | |||
| Rotating trainee | 39.2 (1.9) | 35.1 (1.9) | |||
| Others | 41.6 (1.4) | 34.1 (1.3) | |||
| In which region of KSA are you working? | Central Region | 45.3 (1.7) | 0.000 | 34.8 (2.4) | 0.016 |
| Western Region | 43.0 (1.8) | 36.3 (1.5) | |||
| Eastern Region | 40.3 (2.3) | 35.0 (1.3) | |||
| Northern Region | 38.6 (3.1) | 37.0 (2.8) | |||
| Southern Region | 41.3 (2.3) | 36.3 (1.7) | |||
4. DISCUSSION
This study examined how traumatic stress, psycho- logical well-being, and demographic factors affect healthcare workers. It is hypothesized that HCWs who work in high-stress environments such as emergency, critical care, and ambulance units may experience trauma or distress that can have adverse effects on their mental health and overall well-being. These workers are exposed to various types of stress and trauma that can cause emotional pain and distress, leading to secondary traumatic stress, which can impact their ability to cope and carry out their responsibilities effectively.
The hypothesis of this study is partially accepted as it identified associations among demographic character- istics, traumatic stress, or psychological well-being. Regarding traumatic stress levels, the current study indicated that a significant proportion (80%) of the participants experienced moderate to severe levels of secondary traumatic stress. These findings align with a previous study conducted between July 2021 and July 2022, which reported that approximately 65.4% of HCWs experienced traumatic stress in Saudi Arabia [9]. In line with this study, a recent study by Orrù et al. obtained information on the demographic characteristics and levels of mental distress among healthcare workers from 45 countries [27]. The study found that over 40% of the participants showed signs of moderate to severe secondary traumatization, indicating a high prevalence of this condition among the respondents.
Regarding the association between sociodemographic factors and traumatic stress, the present study found significant differences in secondary traumatic stress scores according to gender, occupation, working unit, and region. Females had higher secondary traumatic stress scores compared to males. Additionally, participants working in the ambulance unit and the emergency department reported higher secondary traumatic stress scores compared to other units [28]. The central region had the highest secondary traumatic stress scores among the regions, further requires more support from the human resource department. Concerning the years of work in specialization and age for secondary traumatic stress scores, analysis could not be performed due to non-normal score distribution.
For psychological well-being, the study found a significant difference in participants' brief inventory of thriving (BIT) scores according to occupation and working unit. This finding is related to previous studies that confirm that health professionals have higher psychological well-being. The HCWs working in palliative care units tend to possess higher levels of psychological resilience [29]. Matua et al. found that healthcare workers in palliative care settings had higher psychological well-being levels than in other healthcare settings [30]. The factors contributing to their well-being included having a supportive work environment, a sense of purpose and meaning in their work, and adequate training and support to manage emotional stress and burnout. The study of Zhang et al. also showed that healthcare professionals who work in palliative care settings experienced high levels of job satisfaction and personal fulfillment [31]. They also reported increased psychological well-being, empathy, and communication skills. On the other hand, the HCWs working in the ambulance unit reported a lower level of psychological well-being which is consistent with a recent study by Mohebbi et al. ambulance workers had a lower level of psychological well-being than the general population [32]. Jennings et al. found that healthcare workers working in ambulances had lower psychological well-being compared to workers in other healthcare settings [33]. This study indicates that potential factors contributing to this phenomenon could be experiencing traumatic incidents, facing excessive work pressure, and receiving insufficient assistance from co-workers and managers.
The findings of high secondary traumatic stress levels and their negative impact on psychological well-being among healthcare workers in this study align with the broader literature on mental health challenges faced by healthcare professionals, particularly during the COVID-19 pandemic. A systematic review and meta-analysis conducted in twenty-one countries reported a high pre- valence of depression (21.7%), anxiety (22.1%), and post-traumatic stress disorder (PTSD) (21.5%) among healthcare professionals during the pandemic [1]. Similarly, Shamsan et al. (2021) [20] found high levels of depression and stress among healthcare workers in Saudi Arabia during the same period. In addition, a literature review conducted by Ulfa et al. [3] showed that traumatic stress was prevalent among healthcare workers globally during the peak of the pandemic, indicating that the negative impact on psychological well-being noted in this study is not limited to healthcare workers in Saudi Arabia but rather a worldwide phenomenon.
Overall, the negative relationship of traumatic stress was found to be a predictor of lower level of psychological well-being. This conceptualization agrees with the evidence that the PWB of healthcare workers is affected by factors such as traumatic stress and sociodemographic characteristics, burnout, and low psychological well-being, as revealed in a systematic review by Van Hoy and Rzeszutek [13], indicated that there is a possibility of the negative influence of traumatic stress on both the mental health and well-being of healthcare professionals. In addition, the mental health symptoms of healthcare workers in this study are congruent with the findings of Pappa et al. [14], a systematic review and meta-analysis of mental health symptoms during the COVID-19 pandemic in Southeast Asia, suggesting that the adverse effects on healthcare workers' mental health are not only present in the context of Saudi Arabia.
4.1. Theoretical Implications
The current study is based on a theoretical component that uses a biopsychosocial model for explaining demographic factors, social factors of traumatic stress, and positive psychology for psychological well-being. This framework has helped to identify connections between these three components, providing a basis for further research in this area. This study also has the potential to become a longitudinal study for tracking the prevalence and factors related to levels of traumatic stress and psychological well-being in healthcare workers. Additionally, qualitative studies should be conducted to understand healthcare workers' experiences and perspectives better [4, 17].
4.2. Practical Implications
HCWs in high-stress environments at hospitals are at risk of experiencing traumatic stress and reduced PWB. Moreover, to support these workers, healthcare organizations must prioritize providing psychological support services. This includes access to mental health professionals, support groups, and other resources that can help HCWs manage their emotional responses to work-related stressors. Hospitals should also implement stress-management programs that provide HCWs with tools and techniques for coping with stress, such as mindfulness training, relaxation techniques, and stress-reduction workshops. In addition, hospital administrators must foster a culture of support that encourages HCWs to seek help when needed. Regular communication, open-door policies, and supportive leadership can all contribute to achieving this. Staffing shortages can contribute to high-stress levels among HCWs, so hospitals should address staffing shortages by implementing policies that ensure adequate staffing levels, reducing the workload for individual HCWs, and providing opportunities for rest and recovery. Finally, healthcare organizations should provide trauma-informed care to patients, recognizing that many patients may have experienced trauma themselves. This can help reduce the likelihood of HCWs experiencing secondary trauma and improve patient outcomes. Overall, by prioritizing the well-being of their HCWs and providing them with the necessary support and resources to manage work-related stress, healthcare organizations can ensure that HCWs can provide the highest quality of care to their patients while maintaining their own PWB. One of the limitations of the current study is related to quantitative measures that can reveal first-hand information related to stress and well-being.
Another hurdle related to the restricted time available to healthcare professionals working in high-stress environments. It delayed the data-gathering process. For further studies, mixed-methods research that combines both quantitative and qualitative methods could be conducted to gain a more comprehensive understanding of the relationship between traumatic stress, PWB, and sociodemographic factors among HCWs in high-stress environments. This approach, such as through in-depth interviews or focus groups, could help identify the complex factors that impact the mental health and well-being of HCWs. Longitudinal studies are recommended to track changes in traumatic stress, PWB, and socio- demographic factors over time among HCWs. This approach could provide insights into the factors that contribute to the development and persistence of mental health issues among healthcare workers. Additionally, comparative studies could be conducted in future research by comparing mental health and well-being of HCWs in high-stress environments, as well as those in low-stress environments or with other groups of workers exposed to high-stress levels, such as emergency responders or military personnel. Comparing these groups could help identify the unique factors that contribute to the mental health of HCWs in high-stress environments and provide insights into potential interventions or support strategies.
CONCLUSION
There is evidence demonstrating that HCWs, especially those working in high-stress environments such as ambulances, suffer from higher STS. Surgeons have a higher psychological wellbeing level as compared to other professionals. The less experienced HCWs have considerably more traumatic stress than their older, more experienced counterparts. HCWs need to be supported and cared for to cope with their work's mental and emotional toll. This can be performed by creating a positive and supportive environment in the hospital. It is essential to alleviate the emotional, cognitive, and physical distress experienced by healthcare workers to boost their motivation and enable them to develop resilience. This will help them to adopt a more positive outlook toward caring for their patients with empathy and kindness.
AUTHOR'S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| PWB | = Psychological Well-being |
| PTSD | = Post-traumatic stress disorder |
| HCW | = Healthcare workers |
| STSS | = Secondary Traumatic Stress Scale |
| BIT | = Brief Inventories of Thriving |
| IRB | = Institutional Review Board |
| SPSS | = Statistical Package of Social Sciences |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study involving survey-based data of human participants was reviewed and approved by [Institutional Review Board of Princess Nourah bint Abdulrahman University (IRB registration number with KACST, KSA: HAP-O1-R-O59]. The study was granted with the letter of exemption status (IRB Log Number: 23-0263).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The participants were provided with written informed consent to participate in this study. All the data gathered were coded to keep the participants' privacy.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the [OSF] at [https://osf.io/sxebj/] and can be shared on request with the author.