All published articles of this journal are available on ScienceDirect.
Self-efficacy and Vaping Behavior among Female Health Students: An Assessment of Health Belief Components
Abstract
Introduction/Objective
Electronic cigarette use (vaping) is an emerging public health concern among young adults. This study examined the prevalence of vaping and its associations with self-efficacy, perceived susceptibility, and perceived severity among female health sciences students.
Methods
A cross-sectional study was conducted among 425 female health sciences students at a university in Riyadh using an online questionnaire.
Results
Eighteen percent of students reported using electronic cigarettes or vaporizers at least once. The number of friends who used electronic cigarettes was significantly associated with students’ vaping behavior (p < 0.05). Among sociodemographic factors, college level (r = -0.121, p = 0.01) and parental education (mother: r = -0.129, p = 0.008; father: r = -0.129, p = 0.008) were negatively correlated with vaping. Self-efficacy was positively correlated with perceived severity (r = 0.300, p < 0.001) and perceived susceptibility (r = 0.265, p < 0.001).
Conclusion
Higher self-efficacy, perceived severity, and perceived susceptibility may reduce the likelihood of vaping among female health sciences students. Awareness programs incorporating self-efficacy and health belief model components are recommended to address vaping behaviors. Additionally, the positive responses of non-users to health belief components highlight the need for workshops on peer pressure and social influence to strengthen students’ ability to resist vaping.
1. INTRODUCTION
Electronic cigarettes pose a growing threat to public health, particularly among young adults. Their sleek designs, appealing flavors, and widespread promotion on social media contribute to a deceptive image that downplays their addictive properties and potential to cause lung damage and cardiovascular problems [1-4]. Electronic cigarettes contain nicotine, flavoring, and various chemicals, several of which can be addictive and harmful to the lungs of both users and bystanders [5, 6]. They are commonly referred to as e-cigs, vape pens, vapes, or tank systems. In 2018, the number of electronic cigarette users in the United States was reported to be 8.1 million, including 1.3 million teenagers [7, 8]. In Saudi Arabia, changing patterns of prevalence, knowledge, and beliefs regarding vaping have been reported over the years. A 2018 study in Saudi Arabia found that 68.9% of adults (aged 18–60 years) vaped, whereas 67% considered it dangerous [9]. One year later, a survey of 1,080 adults (aged 18–74 years) in eastern Saudi Arabia reported a vaping prevalence of 33.6%, whereas 53.8% considered it unsafe [10]. A survey of medical and health sciences college students in Saudi Arabia (aged 18–26 years) found that 27% used electronic cigarettes, nearly twice the prevalence of conventional cigarette smoking [11]. Similarly, a study at the University of Ha’il in Saudi Arabia reported that nearly a quarter of medical and health sciences college students (aged 18–27 years) vaped because of peer pressure [12]. However, higher-quality evidence is needed to better understand the health impacts of e-cigarette use and the role of peer pressure in influencing usage behaviors [13]. Electronic cigarettes are sometimes used alongside tobacco products, as reported among adults in China [14]. Therefore, understanding the reasons behind and patterns of electronic cigarette use is crucial [14]. Most electronic cigarettes contain nicotine and emit dangerous chemicals that can cause lung and cardiovascular diseases [15, 16]. Second-generation vape devices have significantly increased the demand for electronic and combustible cigarettes [4]. Additionally, electronic cigarette use has been associated with adverse effects, including impaired brain development in teenagers, coughing, breathing difficulties, chest pain, nausea, fatigue, fever, and weight loss [17].
Public health professionals play a key role in developing and sharing strategies for addressing electronic cigarette use, which requires an understanding of young users' attitudes and behaviors toward vaping [18-21]. The knowledge, beliefs, attitudes, and behavioral practices of health professional students regarding electronic cigarettes are crucial, as they are responsible for educating patients and staying informed on the latest knowledge. A study among medical students in Saudi Arabia highlighted significant concerns regarding electronic cigarette education, with only 35.1% feeling confident in counseling patients about electronic cigarettes [22], despite reported vaping rates of 12–22% in this population [23, 24]. Moreover, vaping is harmful to pregnant women and their infants. Nicotine in electronic cigarettes restricts the placental blood flow, resulting in low birth weight and premature birth. Additionally, chemicals in electronic cigarettes can cross the placental barrier and affect fetal brain development [25]. Thus, investigating the overlooked relationship between vaping behavior and psychological constructs, such as self-efficacy and behavioral health correlates, among female health sciences students is of significant importance. Bandura introduced self-efficacy as a construct that defines an individual’s beliefs, determining how effectively action plans are implemented in potential situations [26]. Beliefs about self-efficacy significantly contribute to the prediction of intention. Even after controlling for intention, self-efficacy directly influences behavior [27]. Self-efficacy has proven to be effective in motivational and health promotion programs [28]. Additionally, it has been found to correlate with or mediate various smoking cessation programs, primarily in randomized controlled trials where electronic cigarettes were used as an intervention [29, 30].
The Health Belief Model (HBM) is linked to smoking cessation success [31]. A key factor, perceived threat, increases the likelihood of taking action to quit [32, 33]. This perceived threat combines how serious a threat one believes smoking is (perceived severity) and how likely one believes they are to become sick from it (perceived susceptibility) [33]. Individuals who perceive smoking as a serious threat are more likely to attempt quitting smoking and less likely to initiate smoking [31, 34].
In Saudi Arabia, female medical students were found to vape less than male students due to cultural social norms [23]. Therefore, exploring the sociodemographic, psychological, and behavioral correlates of vaping behavior among female medical students is essential for developing prevention strategies based on self-efficacy, perceived susceptibility, and perceived severity for future female health professionals.
This study examined vaping behavior, self-efficacy, perceived susceptibility, and perceived severity among female health sciences students at a university in Riyadh. The selected sample helps address a research gap regarding the unique vaping patterns among female students in Saudi Arabia. While several studies have explored the sociodemographic correlates, prevalence, knowledge, attitudes, and perceptions of Saudi medical students toward vaping, the current study specifically investigated the theoretical implications of the HBM [11, 22-24]. In particular, it examines how self-efficacy, perceived susceptibility, and perceived severity are related to vaping behavior.
Based on the present findings, this study aimed to determine whether the assessment would further include the need to incorporate health promotion campaigns. It was hypothesized that self-efficacy, perceived susceptibility, and perceived severity would correlate with electronic cigarette use among participants.
2. MATERIALS AND METHODS
2.1. Study Design
This cross-sectional, descriptive, and correlational study examined vaping behavior, self-efficacy, perceived susceptibility, and perceived severity among health sciences students at a university in Saudi Arabia. The study was conducted within a defined timeframe from January 5, 2021, to April 6, 2021. This university was selected as the study setting because of its diverse and representative population of female health sciences students.
2.2. Sample and Study Population
The target population comprised female health sciences students enrolled at a university in Riyadh. The sample size was determined using the following formula:
 |
where n represents the required sample size, Z is the standard normal deviation at a 95% confidence level (1.96), p is the estimated proportion of the characteristic under study (set at 0.5 to ensure maximum variability), q is calculated as 1−p1 - p1−p, d denotes the margin of error (0.05), and N refers to the total student population (6,500). Based on this formula, the estimated sample size was 363 participants. However, due to a higher-than-expected response rate, 425 students ultimately participated in the study.
Eligible participants were students actively enrolled in a health sciences program. To ensure a comprehensive assessment of vaping behavior, individuals who had used vapes, traditional cigarettes, cigars, or shisha were included. Students from non-health programs were excluded to maintain the focus of the study.
2.3. Conceptual Framework
The HBM is a widely used theoretical framework in health behavior research, particularly in smoking cessation and substance use prevention. The model suggests that individuals' likelihood of engaging in or avoiding health-related behaviors depends on their perceived susceptibility (how vulnerable they feel about the negative health effects of vaping) and perceived severity (how serious they believe these health risks are). Previous research indicates that individuals who perceive greater health risks associated with vaping are less likely to engage in the behavior and more likely to attempt cessation [31, 34].
2.4. Measures
The participants were recruited through an online survey (Google Forms) distributed via student groups. The questionnaire consisted of 21 items divided into four sections. The sociodemographic information section included seven items covering age, college program, semester level, parental education level, residence, and monthly stipends. The electronic cigarette use and vaping behavior section comprised five items assessing vaping status, type of electronic cigarette used, duration of use, presence of family members who vape, and number of friends who vape. The perceived threats section contained six items, with three assessing perceived susceptibility and three evaluating perceived severity, to measure students' perceptions of vaping-related risks. Finally, the self-efficacy section included three items measured on a 5-point Likert scale (ranging from 1 = Strongly Disagree to 5 = Strongly Agree) to assess students’ confidence in resisting vaping.
2.5. Validity and Reliability
A pilot study involving 30 health sciences students was conducted to evaluate the clarity, reliability, and cultural sensitivity of the questionnaire. Based on participant feedback, modifications were made to enhance comprehension and accuracy. Specifically, financial-related items were clarified by changing “your monthly income” to “your stipend (not your family income),” ensuring a more precise interpretation. In addition, vaping-duration response options were refined to eliminate ambiguity. The internal consistency of the questionnaire was assessed using Cronbach’s alpha, which yielded a reliability coefficient of 0.7213, indicating an acceptable level of reliability for exploratory research.
2.6. Data Analysis
Data analysis was conducted using the JMP software (version 16; SAS Institute Inc., Cary, NC, USA). Descriptive statistics, including frequencies, means, and standard deviations, were used to summarize demographic and behavioral variables. Normality tests were performed to determine the appropriate statistical methods. Correlation and regression analyses were conducted to examine the relationships among vaping behavior, self-efficacy, and perceived susceptibility/severity. Statistical significance was set at p ≤ 0.05. The dataset is publicly available in the research repository (https://osf.io/6t95j) and can be shared upon request.
2.7. Ethical Considerations
This study was approved by the Institutional Review Board (IRB) of Princess Nourah University (IRB Log: 21-0004) and was exempted from full review. Informed consent was obtained electronically before participation, and participants were explicitly informed of their right to withdraw at any time without any consequences. Confidentiality and anonymity were strictly maintained, ensuring that no identifying information was linked to responses. All data were stored securely and used exclusively for research purposes.
2.8. Role of the Health Coach/health Educator/health Education Specialist
The key researchers in this study included certified health education specialists, health education students, and a clinical psychologist. The findings of this study align with several priority areas outlined by the National Commission for Health Education Credentialing [35]. In Area 1, Assessment of Needs, competency 1.1 (assessment planning) was applied, with sub-competency 1.1.2 identifying the priority population of female health students to assess the prevalence of vaping behavior. Sub-competency 1.1.4 examined factors and determinants influencing the assessment process by developing a sociodemographic information sheet, whereas sub-competency 1.1.5 ensured recruiting a priority population of health sciences students to participate in the assessment. Competency 1.2 was used to obtain primary data, with 1.2.1 identifying primary data; 1.2.7 used for data collection needs, instruments, methods, and procedures; and 1.2.8 ensuring adherence to established procedures of data collection. Competency 1.3 was applied for data analysis, with sub-competencies 1.3.2 and 1.3.3 analyzing self-efficacy; perceived susceptibility; perceived severity beliefs; vaping behaviors; and social, cultural, and economic factors that impact the health of the priority population. The competency of synthesizing assessment findings (1.4) was fully utilized for comparison with existing data (1.4.1), prioritizing (1.4.2) and summarizing health promotion needs (1.4.3) by providing recommendations (1.4.4) and reporting findings (1.4.5).
| Variables | Shapiro–Wilk | |
|---|---|---|
| Statistic | Sig. | |
| Demographic Information | - | - |
| Age | 0.929 | 0.000 |
| College | 0.778 | 0.000 |
| College Level | 0.882 | 0.000 |
| Mother’s Education | 0.845 | 0.000 |
| Father’s Education | 0.844 | 0.000 |
| Residence | 0.498 | 0.000 |
| Vaping Behavior: Personal | - | - |
| Do you use vapes? | 0.462 | 0.000 |
| If you use, what type do you use? | 0.941 | 0.002 |
| For how long have you used vapes? | 0.811 | 0.000 |
| Vaping Behavior: Significant others | - | - |
| Family member who uses | 0.772 | 0.000 |
| Number of friends who use | 0.714 | 0.000 |
| Perceived Severity | - | - |
| The earlier a person starts vaping, the greater the harm | 0.736 | 0.000 |
| Vapers are more likely to get sick than non-vapers | 0.866 | 0.000 |
| Vapers die earlier than non-vapers | 0.888 | 0.000 |
| Perceived Susceptibility | - | - |
| I will become addicted if I vape | 0.883 | 0.000 |
| I would get sick if I vape | 0.849 | 0.000 |
| If I vape, I may die earlier | 0.866 | 0.000 |
| Self-efficacy | - | - |
| No one could persuade me to try vaping | 0.728 | 0.000 |
| Even if all who are around me vape, that does not mean I must vape | 0.596 | 0.000 |
| I can refuse even if a friend or relative encourages me to vape | 0.619 | 0.000 |
In Area II, a questionnaire was developed for surveying (2.4.2), and alternative actions were planned to address potential challenges (2.4.3). Area IV involved using sub-competency 4.2.1 to determine the purpose and hypothesis and ensure compliance with IRB (4.2.2). Self-efficacy and HBM components were incorporated (4.2.3), and a sampling plan and procedures for data collection, management, and security were developed (4.2.6). Instruments for collecting data were adapted (4.2.8). Moreover, data collectors (4.3.1) were trained, data collection procedures were implemented (4.3.2), and online survey forms were utilized. Responses were saved in an Excel data sheet and SPSS after coding, followed by statistical analyses (4.3.3, 4.3.5, and 4.3.6). All sub-competencies of 4.4 were applied for data analysis. Within Area V, Advocacy, sub-competency 5.1.3 was used to identify factors that facilitate and/or hinder advocacy efforts. Findings indicated that age, self-efficacy, perceived severity, or perceived susceptibility were associated with a decrease in the possibility of student vaping, whereas a unit increase in stipend was associated with an increase in the possibility of vaping.
3. RESULTS
3.1. Demographic Characteristics of the Study Participants
All variables in this study followed a normal distribution, as the p-value of the Shapiro–Wilk test yielded a value of 0.000, less than the alpha level of 0.05, at a 95% confidence interval (Table 1).
The demographic characteristics of the participants are presented in Table 2. Participants’ ages ranged from 18–26 years (20 ± 1.4). Electronic cigarette use was the most common among students in the College of Health and Rehabilitation Sciences (n = 25; 36.23%). The second-highest rate of prior electronic cigarette use (either once or multiple times) was observed among students in the College of Nursing (27.54%, n = 19). Furthermore, 36.22% (n = 25) of the students who used electronic cigarettes were in college level 5 to 6.
| Demographic Characteristics | Electronic Cigarette Ever-users n (%) | Electronic Cigarette Never-users n (%) | Total n (%) |
|---|---|---|---|
| or M ± SD | or M ± SD | or M ± SD | |
| Age | 0.5 ± 0.06 | 20.14 ± 1.38 | 20.19 ± 1.44 |
| College | - | - | - |
| Preparatory year | 14 (20.29%) | 101 (28.37%) | 115 (27.05%) |
| College of Medicine | 4 (5.80%) | 14 (3.93%) | 18 (4.23%) |
| College of Nursing | 19 (27.54%) | 54 (15.17%) | 73 (17.17%) |
| College of Pharmacy | 7 (10.14%) | 21 (5.90%) | 28 (6.58%) |
| College of Dental | 0 (0%) | 2 (0.56%) | 2 (0.47%) |
| College of Health and Rehabilitation Sciences | 25 (36.23%) | 164 (46.07%) | 189 (44.47%) |
| College Level | - | - | - |
| Levels 1 to 2 | 15 (21.73%) | 110 (30.90%) | 125 (29.41%) |
| Levels 3 to 4 | 4 (5.80%) | 56 (15.73%) | 60 (14.11%) |
| Levels 5 to 6 | 25 (36.22%) | 90 (25.28%) | 115 (27.05%) |
| Levels 7 to 8 | 18 (26.1%) | 80 (22.47%) | 98 (23.05%) |
| Levels 9 to 10 | 0 (0%) | 4 (1.12%) | 4 (0.94%) |
| Levels 11 to 12 | 2 (2.90%) | 2 (0.56%) | 4 (0.94%) |
| Internship year | 5 (7.25%) | 14 (3.94%) | 19 (4.47%) |
3.2. Prevalence of Electronic Cigarette Use among Health Students
Table 3 presents the frequency of vaping among health sciences students. “Yes” denotes the number of students who had used electronic cigarettes, and “No” denotes the number of students who had not. Nearly half (45%; n = 34) of the participants had previously used electronic cigarettes, whereas 32% (n = 24) reported use within the past three months.
| Behavior | N | % |
|---|---|---|
| Do you use vapes? | ||
| No | 350 | 82% |
| Yes (either once or multiple times) | 75 | 18% |
| Type of vaping? | ||
| E-cigarettes with or without tobacco | 75 | 100% |
| E-cigarettes with traditional cigarette | 30 | 40% |
| E-cigarette with Cigar | 10 | 13% |
| E-cigarette with Shisha | 35 | 47% |
| How long did you use vapes? | ||
| Current use for 1-3 month(s) | 11 | 15% |
| Ever-use (tried it before) | 34 | 45% |
| More than 3 months | 24 | 32% |
| Never used vapes (shisha only) | 6 | 8% |
3.3. Correlations with Family Members and the Number of Friends who Use Electronic Cigarettes
Binary logistic regression indicated no significant association between students’ vaping behavior and family members who used vapes (p > 0.05). In contrast, the number of friends who used electronic cigarettes was significantly associated with students’ vaping behavior (p < 0.05). The odds ratios (ORs) are shown in Table 4. All levels above “none” showed significant ORs above 1, indicating that as the number of friends who vape increases, health sciences college students are more likely to vape. Fig. (1) illustrates this trend, showing a higher proportion of electronic cigarette users among students with 1–2 and 3–4 friends who vape.
| Level | OR | 95% CI | p |
|---|---|---|---|
| 1 or 2 | 10.813 | (4.487-26.059) | < 0.001* |
| 3 or 4 | 52.714 | (20.582-135.013) | < 0.001* |
| 5 or more | 82 | (24.302-276.683) | < 0.001* |
3.4. Relationship between Sociodemographic Variables and Vaping Behavior
Pearson’s correlation analysis between sociodemographic variables (age, college program, college level, mother’s education, father’s education, residence, and monthly stipend) and vaping behavior showed that college level (r = -0.121, p = .01), mother’s education (r = -0.129, p = .008), and father’s education (r = -0.129, p = .008) were significantly negatively correlated with vaping (Table 5). This implies that students with higher parental education levels and those in higher college levels were less likely to vape.
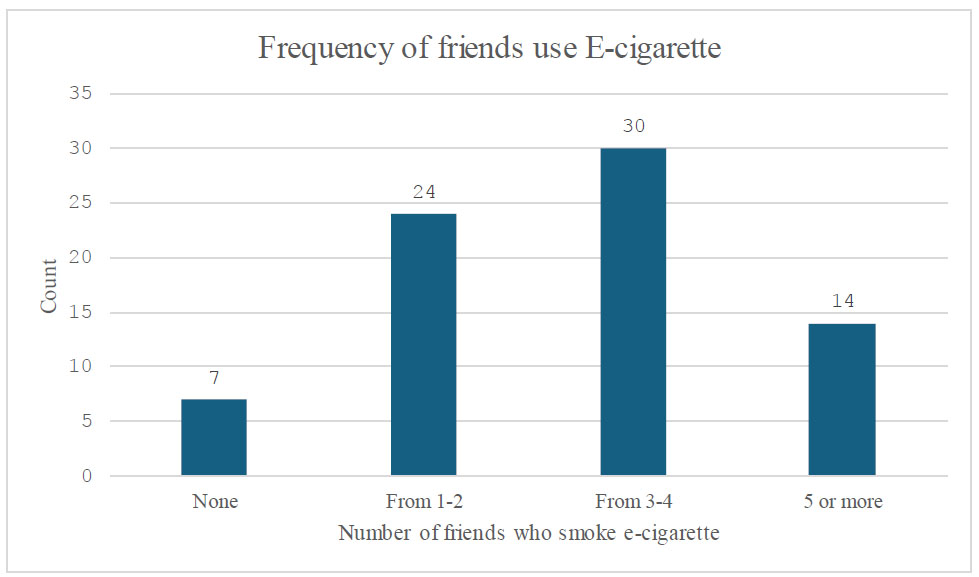
Frequency of electronic cigarette users across different categories based on the number of friends who use electronic cigarettes. Abbreviation: E-cigarette; electronic cigarette.
| Variables | Age | College | College Level | Mother’s Education | Father’s Education | Residence |
|---|---|---|---|---|---|---|
| Vaping | -.075 | -.001 | -.121* | -.129* | -.129* | .028 |
3.5. Correlations between Self-efficacy, Health Belief Components, and Vaping Behavior
Pearson’s correlation coefficients revealed associations between self-efficacy, perceived severity, perceived susceptibility, and vaping behaviors. A weak positive correlation was observed between self-efficacy and perceived severity (r = 0.300, p =0.00) and between self-efficacy and perceived susceptibility (r= 0.265, p = 0.000). A moderately positive correlation was observed between perceived severity and susceptibility (r = 0.458, p = 0.000). However, vaping behavior did not significantly correlate with self-efficacy or health belief components (Table 6).
| Variables | Self-efficacy | Perceived Severity | Perceived Susceptibility |
|---|---|---|---|
| Perceived Severity | .300** | - | - |
| Perceived Susceptibility | .265** | .458** | - |
| Vaping Behavior | -.013 | -.005 | -.006 |
| - | B | S.E. | Wald | df | Sig. | Exp(B) |
|---|---|---|---|---|---|---|
| Step 1a Self-efficacy | -.003 | .630 | .002 | 1 | .963 | .997 |
| Perceived Severity | -.019 | .067 | .078 | 1 | .780 | .982 |
| Perceived Susceptibility | -.029 | .059 | .233 | 1 | .629 | .972 |
| Age | -.020 | .099 | .040 | 1 | .842 | .980 |
| Stipend | .000 | .000 | 3.030 | 1 | .082 | 1.000 |
| Constant | 2.703 | 2.108 | 1.644 | 1 | .200 | 12.924 |
3.6. Effects of Age, Stipend, Self-efficacy, Perceived Severity, and Perceived Susceptibility on the Likelihood of Vaping
Binary logistic regression was performed to determine the effects of age, stipend, self-efficacy, perceived severity, and perceived susceptibility on the likelihood of vaping among students. The logistic regression model was not statistically significant, X2(8) = 3.710, p = 0.882. The model explained 2.7% (Nagelkerke R2) of the variance in vaping, and correctly classified 82% of the cases. As shown in Table 7, none of the independent variables (age, stipend, self-efficacy, perceived severity, and perceived susceptibility) was statistically significant as an influencing factor for students’ vaping behavior. Column (B) shows that a unit increase in age, self-efficacy, perceived severity, or perceived susceptibility was associated with a decrease in the possibility of vaping, whereas a unit increase in stipend was associated with an increase in the possibility of vaping.
4. DISCUSSION
Vaping is a rapidly growing global public health concern among young adults. Given the increasing use of electronic cigarettes in many countries, understanding them as a novel phenomenon is essential. However, few studies have specifically examined female health students, who are expected to recognize the health risks associated with electronic cigarette use. This study aimed to assess self-efficacy and its relationship with key HBM components, including perceived severity and susceptibility to electronic cigarettes, among health sciences students. The findings partially supported the hypothesis. Although self-efficacy, perceived severity, and perceived susceptibility were interrelated, they did not directly influence vaping behavior. Several factors may account for this inconsistency, including social, environmental, and situational influences, such as peer pressure, the normalization of vaping among youth, and the novelty and accessibility of electronic cigarettes, which may further create resistance toward behavioral change. Among environmental factors, the availability and marketing of electronic cigarettes, as well as the role of media or social media in promoting vaping, play a significant role. Certain sociodemographic factors, such as the number of friends who use electronic cigarettes, were found to be significantly associated with vaping behavior, reinforcing previous findings [12]. Simultaneously, certain protective factors within sociodemographic variables emerged as protective factors against vaping, aligning with existing literature on resistance to vaping behavior. One such factor is related to senior-level students who are less likely to engage in vaping. Previous studies support these findings, indicating that maturity and knowledge play a protective role against vaping, as well as novelty and sensation-seeking behaviors [3]. Another protective factor is parental education, which is negatively related to vaping behavior [36].
The negative correlation between higher college level and vaping behavior may be attributed to multiple factors. First, senior students typically have greater exposure to health-related coursework and professional training, particularly in health science programs, which enhances their awareness of the risks associated with vaping. Second, increased maturity and life stability at advanced college levels may contribute to more health-conscious decision-making and a reduced likelihood of engaging in risky behaviors, such as vaping. These findings align with previous research suggesting that as students progress through their academic careers, they become more inclined to prioritize long-term health over short-term social trends [37]. Additionally, senior students may experience less peer pressure, as their social circles often shift toward academic and professional networks, which discourages risky behaviors such as vaping.
The observed negative correlation between parental education and vaping behavior suggests that higher parental education levels may contribute to more health-conscious parenting styles and stronger communication regarding the risks of substance use. Educated parents are more likely to emphasize preventive health behaviors, provide accurate health information, and model healthy lifestyle choices, which may reduce the likelihood of their children engaging in vaping [36]. Furthermore, higher parental education is often associated with greater socioeconomic stability, which reduces stressors that may drive students toward risk-taking behaviors, including vaping. This aligns with the findings of Jaffar et al. [37] who reported that socioeconomic and educational backgrounds play critical roles in shaping youth perceptions of vaping risks.
Approximately 425 health science college students, with a mean age of 20 years, participated in this study. The prevalence of vaping behavior among female health sciences students was 18%. This may be attributed to companies that advertise and market electronic cigarettes and the fact that these devices are now more readily available. These factors may lead to a high rate of intentional behavior. This finding is in contrast with those of previous studies [11, 22]. In 2017, 27% of health sciences students in Jeddah reported using electronic cigarettes, which was higher than that reported in this study [11]. A study from Alfaisal University conducted in 2020 reported that females were less likely to use electronic cigarettes than men; however, the prevalence among females in that study (12.2%) was lower than that in the present study [23].
Moreover, the majority of participants who reported vaping were from the College of Health and Rehabilitation Sciences, which may be attributed to the college’s proportionately larger size than other health colleges (comprising 13 academic programs and more than 1500 students out of a total of 5000 students in health sciences colleges). Furthermore, in the current study, most participants who used vapes were in college levels 5–6. This suggests that the novelty that students experienced during the lower levels of college may increase the likelihood of experimenting with vaping, whereas the senior levels are more demanding, which discourages vaping. A long-term study conducted by the University of Michigan reported a decline in vaping rates among adolescents as they age. This trend can also be observed in medical schools. In this context, smoking/vaping cessation programs/clinical awareness programs, as well as workshops on life skills, can help young adults overcome undesirable behaviors [31, 38].
Approximately one-quarter of students who reported vaping had one or two friends who also vaped, suggesting that peer influence, conformity, and curiosity may have contributed to their behavior. Similar outcomes have been previously reported [12, 24, 38]. Regarding the sociodemographic correlates of vaping behavior, higher college and parental education levels were negatively correlated with vaping. Students at a higher college level are typically more mature, knowledgeable, and educated about healthy behaviors. Various course modules are available for health students, such as Health Behavior, Society and Health, Human Behavior, Introduction to Health Determinants, Mental Health, and Substance Abuse. Jones et al. [3] posited that knowledge of harmful behaviors could decrease vaping behaviors.
Furthermore, the role of parents in shaping behavioral development cannot be overlooked [3]. Higher parental education can positively affect children’s behaviors. Consistent with this, previous research has reported a negative correlation between maternal education and vaping behavior [39]. Self-efficacy plays a significant role in preventing vaping behaviors. More than half of the participants strongly agreed with the statement, “No one could persuade me to try vaping,” indicating a high level of self-efficacy among the students [3]. This finding can be linked to increased self-protective behavior against vaping. This is consistent with a previous study that found a low probability of trying electronic cigarettes among respondents who had never used them [40].
Furthermore, one-quarter of the participants expressed a neutral stance on the statement, “I will become an addict if I vape electronic cigarettes.” In contrast, a study conducted in Saudi Arabia reported that nearly half of the participants perceived vaping as less addictive than traditional cigarette smoking [9]. This difference in perceived addictiveness may stem from the belief that electronic cigarettes help users quit smoking. Moreover, over one-third of the participants strongly agreed with the statement, “I would get sick if I vape,” likely due to their awareness of vaping-related harmful effects, such as cancer. Similarly, in the aforementioned Saudi Arabian study, more than half of the participants believed that electronic cigarettes were unsafe; however, they were considered less dangerous than traditional cigarettes [9]. Over one-third of the participants strongly agreed with the statement, “If I vape, I may die earlier,” possibly reflecting their belief that electronic cigarettes contain harmful substances similar to those in tobacco cigarettes. In contrast to the current findings, 23% of university students perceived electronic cigarettes to be less harmful than tobacco cigarettes [41]. In this study, half of the respondents (56%) strongly agreed with the statement, “The earlier a person starts vaping, the greater the harm.” Higher levels of education and knowledge strengthen this belief. Therefore, respondents were familiar with the product and recognized the effects of vaping on their health. Consistent with this, a study in the Aljazan region of Saudi Arabia reported that the majority of undergraduate students perceived that exhaled vapor from electronic cigarettes could adversely affect their health [42]. Moreover, in an Austrian study, most surveyed students believed that electronic cigarettes damaged their health [43].
Finally, although the regression model yielded insignificant results, it predicted that age, self-efficacy, perceived severity, and perceived susceptibility were associated with a decreased likelihood of vaping, whereas a higher student stipend was linked to an increased likelihood. This indicates that self-efficacy and HBM-based programs can promote healthy behaviors among students. However, knowledge of risk alone is insufficient to prevent addictive behaviors [36]. Participants in this study were not enrolled in any treatment program. Other significant mediating factors, such as self-control and self-regulation, may influence the relationship between HBM components and vaping behavior [44] and should be examined in future research. Additionally, the Theory of Planned Behavior could serve as an alternative framework for a deeper exploration of psychological factors that contribute to behavioral change.
5. STUDY LIMITATION
This study has some limitations that should be addressed in future research. Treatment-related factors and vaping cessation attempts, which are essential for understanding quitting behaviors and the challenges individuals face, were not explored. Additionally, further investigation into psychological and social motivators, such as pleasure, sensation-seeking, and curiosity, could provide deeper insights into vaping behavior. As the current study is correlational, future longitudinal or experimental research is required to explore potential causal relationships. Moreover, qualitative methods, such as focus groups, could help uncover the underlying attitudes, motivations, and social influences related to vaping behavior.
A key limitation of this study is its focus on a single university in Saudi Arabia, which may not fully represent broader national or international populations of university students. These findings specifically reflect the vaping behaviors and perceptions of female health sciences students, leaving uncertainty about whether similar trends apply to male students or those from other academic disciplines. Additionally, cultural and institutional differences across universities may shape vaping attitudes and behaviors. To enhance external validity, future research should include multiple universities, a wider range of academic disciplines, and male students to determine whether these patterns persist across different cultural settings.
CONCLUSION
This study found that 18% of female health science students reported vaping, with peer influence being a significant factor in their behavior. Although self-efficacy, perceived severity, and perceived susceptibility were positively correlated, they did not show a direct association with vaping behavior. However, higher college level and parental education were negatively correlated with vaping, suggesting that maturity and knowledge may serve as protective factors.
These findings emphasize the need for targeted health education interventions that strengthen self-efficacy and perceived threat to reduce vaping among students. Prevention strategies should address peer influence, social norms, and misconceptions regarding vaping-related health risks. Health education specialists and psychologists can play key roles in designing awareness campaigns, smoking cessation programs, and behavioral interventions tailored to young adults. Future research should explore additional psychological and environmental factors influencing vaping, including social media exposure, stress, and self-regulation strategies. Additionally, expanding the study population to include male students, students from different universities, and individuals from diverse cultural backgrounds is essential for understanding the broader applicability of these findings and strengthening their external validity.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: A.A., U.Z.: Writing - Reviewing and Editing; S.A.: Conceptualization; T.A., N.M.: Data Collection. All authors reviewed the results and approved the final version of the manuscript.
ABBREVIATION
| HBM | = Health Belief Model |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Institutional Review Board (IRB) of Princess Nourah University, Saudi Arabia (IRB Log: 21-0004).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained electronically before participation, and participants were explicitly informed of their right to withdraw at any time without any consequences.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
The authors thank all participants for their valuable participation.