All published articles of this journal are available on ScienceDirect.
The Development of Virtual Reality Exposure Therapy (VRET) for Young Adults in Russia and Indonesia
Abstract
Introduction
Mental disorders, particularly depression and anxiety, are prevalent in Russia and Indonesia. While mental health services are widely accessible in Russia, Indonesia faces challenges such as limited professionals and stigma. Early adults (18-40 years) often experience mental disorders in both countries. Latest technologies, such as Virtual Reality Exposure Therapy, offer potential solutions by helping individuals confront fears in a controlled, therapist-guided environment, and overcome the limitations of conventional therapy. Therefore, it is notable to evaluate the current development and utilization of this technology.
Methods
Using the Literature Review method, a literature search was conducted in several databases, including DOAJ, PsycInfo, PubMed, and Scopus, focusing on empirical studies published from 2015 to 2024. Inclusion and exclusion criteria were applied to screen and select relevant studies for analysis.
Results
Virtual Reality Exposure Therapy is effective in treating mental disorders among early adults in both countries. It is also found that Virtual Reality Exposure Therapy is used as a tool to assess the initial evaluation of the client's mental condition. The study also noted variations in the types of Virtual Reality Exposure Therapy devices used in Russia and Indonesia, indicating differences in technological utilization.
Conclusion
Virtual Reality Exposure Therapy is a promising and innovative method for addressing mental health problems both in Russia and Indonesia. While there are differences in technologies between these countries, its success relies on integration with clinical practices and proper therapist training. Further research is needed to better understand the full potential of Virtual Reality Exposure Therapy in addressing this troubling mental health issue.
1. INTRODUCTION
Mental disorders are a common and crucial problem in various countries, including countries with high populations like Russia and Indonesia. In 2018, it was recorded that there were 379,818 patients with an initial diagnosis of mental disorders who sought counseling and psychological intervention services in Russia. This number shows an increase of around 3.4% from 2017 [1]. Depression and anxiety are the most common mental disorders in Russia. There is a significant difference between the number of people who have symptoms of depression and anxiety and the number of people who have reported that they have been diagnosed and seek professional treatment for the disorders [2, 3]. Meanwhile, in Indonesia, a survey from the Global Health Data Exchange in 2017 found that 27.3 million people in Indonesia experienced mental health problems, indicating that one in ten people in the country suffers from mental disorders [4]. The results of the 2018 Riskesdas (Basic Health Research) also show that more than 19 million Indonesians aged over 15 years experienced mental and emotional disorders [5]. Additionally, more than 12 million people in the same age group experienced depression. The existence of mental health services in these two countries is very necessary considering the high prevalence of mental disorders and the large population in both countries.
Hurlock explained that early adulthood is individuals aged between 18 and 40 years [6]. Mental health problems are quite common in early adulthood, where by the age of 18, around 15.5% of individuals have experienced various types of mental disorders, such as anxiety, depression, and substance abuse [7-9]. Anxiety is a condition when an individual feels very worried, nervous, or afraid of everyday situations. Anxiety disorders are commonly affecting approximately 9.6% of men and 26.7% of women in their 20s. Major Depressive Disorder (MDD) is also a considerable mental health problem seen in 4.4% of men and 7.2% of women in their 20s. This disorder is characterized by feelings of sorrowfulness, hopelessness, and lack of interest [10]. This shows the importance of attention to psychological services for early adulthood populations.
Health education and development should focus on addressing mental health stigma and mental health literacy. However, culturally, this has hardly been explored in recent Russia [11]. Currently, the Russian government is making efforts to provide psychological services. The government of Russia already provides various mental health services and social support for individuals with mental disorders. These services, including emergency counselling, diagnostics or assessment, treatment, psychological prevention, and rehabilitation, are available for both inpatient and outpatient facilities. The provided facilities are located close to where patients live to ensure that services are easily accessible to those who need them [12-14]. Mental health care in Indonesia faces many problems, such as a shortage of mental health professionals, lack of funding, and a large disparity between the number of people who need treatment and those who actually receive it. This challenge is happening in rural and suburban areas, where knowledge about mental health is still lacking, and a stigma towards mental health problems, which they consider as a taboo [15-17]. The various approaches taken by Russia focus more on how autonomy or independence is formed and developed during the process, while foreign approaches focus more on the final results or achievement of autonomy itself [18]. This can be seen from the various developments in psychological interventions that have been developed by Russia and will continue to develop in various fields of psychology.
It is undeniable that the global COVID-19 pandemic is also one of the causes of mental disorders, especially among young adults [19-23]. This impact can be seen from research on university students in Russia during the pandemic, which shows that their level of psychological well-being has not changed much compared to normal conditions. However, mental health indicators such as depression, anxiety, and stress have increased significantly, indicating the presence of more specific mental health problems even though their general psychological well-being remains stable [24]. Apart from that, each country also faces unpleasant situations related to natural disasters, such as tsunamis, floods, and earthquakes in Indonesia, and artificial disasters that have a significant impact on mental health. It is shown that Internally Displaced Persons (IDPs) have higher psychological distress compared to non-refugees. This shows the effect of the long-term impact of those traumatic events on mental well-being, even in secluded areas [25]. Based on these two situations, we could witness the long-term mental health consequences of traumatic events and emphasize the need for a comprehensive and effective support system to fulfill the mental health necessities of those who are affected by the war conflict and disasters in both countries.
Aside from the situations mentioned above, in both Indonesia and Russia, many people have caregiver duties at home. They care for their family members indefinitely, so this work requires physical and even psychological energy. Physically, caregivers should have good physical health and stable mental health in order to provide optimal care [26].
Summarizing the above passage, considering the large populations of the two countries and the challenges they face, it is necessary to explore various approaches to mental health treatment. So far, exposure therapy has always been considered the main foundation of Cognitive Behavioral Therapy (CBT) in the treatments for anxiety [27-30]. However, based on the reports from the service providers, the use of exposure therapy to treat adults with anxiety disorders is rather infrequent compared to other CBT approaches like relaxation techniques or cognitive [31-33]. Exposure therapy includes a variety of psychological interventions or psychotherapy techniques commonly aimed at overcoming pathological fears in individuals with anxiety disorders [34]. Although generally categorized under CBT, this therapy can also be used to reduce pathological fears unrelated to anxiety disorders [35].
Although the emphasis of exposure therapy may vary based on the psychological disorder being treated, this intervention usually consists of several key components. First, specific goals of therapy are established through collaboration between therapist and client. They outline practice goals in terms of duration or target behavior described in clear, measurable terms. Second, therapists explain possible negative consequences, helping clients identify feared outcomes associated with a given task [36]. Strong evidence supports the effectiveness of exposure therapy in treating anxiety disorders, including specific phobias, panic disorder, obsessive-compulsive disorder, and post-traumatic stress disorder [37-39]. In this context, the term “effectiveness” refers to the ability of exposure therapy to relieve symptoms and effectively manage anxiety disorders.
Most technological developments in this day have entered the era of digitalization, where almost all aspects of human life are essentially affected by digitalized technology, such as education, communication, entertainment, business, and even in treatment of mental disorders. Types of digital interventions commonly used to treat mental disorders include telemedicine, mobile medical applications, virtual reality applications, digital therapeutics, and digital biomarkers [40-44]. Exposure therapy now uses various digital technologies that make it easier for therapists and clients to treat various mental disorders. Digital intervention in exposure therapy involves the use of technology to deliver Cognitive Behavioral Therapy for anxiety disorders such as specific phobias and Obsessive-Compulsive Disorder (OCD). Research shows that digital tools such as virtual reality serve as powerful tools in the 4.0 Industry era. When combined with traditional therapeutic methods, this technology offers an effective approach to treating a range of mental health conditions [45].
Although traditional exposure therapy has been shown to be effective in treating anxiety disorders, it has various limitations. Some of these limitations include limited control over the situation, challenges in maintaining confidentiality during direct exposure (in vivo), logistical obstacles in accessing the necessary stimuli, and financial and time constraints for clients and therapists. There is difficulty in imitating certain situations and client reluctance to engage in treatment [46, 47]. In response to these weaknesses, Cognitive Behavioral Therapy (CBT) has evolved to incorporate imaginary exposure with the integration of high technologies, leading to the development of Virtual Reality Exposure Therapy (VRET) as an effective and more practical alternative to traditional or in vivo exposure therapy [48]. Although traditional exposure therapy has shown effectiveness, it is not used consistently due to the discomfort and intimacy experienced by patients, even with their therapists [49]. VRET is equivalent in effectiveness to traditional CBT approaches but offers additional advantages such as increased accessibility, safety, and acceptability by patients and therapists. This makes VRET an important method in the present day in the treatment of anxiety disorders and other psychological conditions [50-52].
Virtual Reality (VR) Exposure Therapy is a form of computer-based intervention that utilizes virtual reality technology to help individuals overcome and treat complex problems of mental disorders. In VR, users are involved in a computerized interactive environment, where they can feel the presence of and live interaction with virtual objects, subjects, and situations. Users generally wear a head-mounted VR equipped with a screen in front of each eye, headphones, and position trackers to adjust the virtual visualization according to their physical movements in real time. Some VR applications may require the use of a handheld device, such as a joystick for navigation within the virtual environment and operating buttons in a virtual elevator or driving a virtual car [53].
Virtual Reality (VR) technology allows the real-world environment to be replaced with a simulated virtual world that replicates specific situations, particularly those that trigger anxiety disorders. VRET expands the possibilities of traditional exposure therapy by increasing user acceptance, providing greater monitored control, and allowing access to situations that are difficult or impossible to access in real-world environments in conventional therapy [54]. Virtual environments can be designed by therapists to display a realistic environment, although they may lack some of the natural details encountered in the real world. The more realistic the virtual environment, the stronger the feeling of immersion or “presence” felt by the participant. Unlike the real environment, the virtual environment gives researchers the capability to fully control every aspect of a scene, including the behavior or movements of the avatar which are difficult to do in real life considering the huge amounts of variables that could unexpectedly change. The virtual reality system enables an accurate measurement of the movements and reactions of an individual, including even the movements of the head and body [55].
Virtual Reality Exposure Therapy (VRET) uses virtual reality technology to simulate exposure to feared objects or situations within a fully controlled environment. This therapy incorporates the principles of exposure therapy with virtual reality technology to construct a realistic and interactive three-dimensional environment [56]. VRET offers several advantages, including the accessibility of virtual reality devices and the ease with which individuals can receive the therapy. These convenient advantages make VRET a potential solution in treating the high prevalence of mental health disorders in both Russia and Indonesia, where both countries also have great potential in developing VRET even further. Therefore, we reviewed various literatures of VRET research that were done in Russia and Indonesia to obtain information about the development and utilization of VRET in both countries.
2. METHODS
A literature review was used to synthesize the scientific proofs that were found. The study was carried out using three main steps. The first step was to search for various keywords to obtain specific literature. The second step was to assess the obtained literature using the Downs & Black Checklist [57]. The third step was to synthesize and summarize the results.
A literature search was conducted in databases of DOAJ, PsycINFO, PubMed, and Scopus on May 19th, 2024, with the publication year set between 2015 and 2024. To ensure relevance to the research topic, the keywords determined were “VRET,” “Virtual Reality Exposure Therapy,” and “Mental Disorders”. The inclusion criteria used were full-text articles resulting from experimental research conducted in Russia or Indonesia, with early adult participants aged 18-40 years. Meanwhile, exclusion criteria included gray literature, articles that are not relevant to the keywords, and theoretical reviews. The selected literature will be assessed using the Downs and Black Checklist [57] to critically evaluate the quality of the quantitative research methodology of each selected article. The checklist contains 28 items that were used to assess the obtained literature, which contains various assessment components, such as reporting, external validity, internal validity, and power. The scores were categorized into four types: poor (≤14), fair (15-19), good (20-25), and excellent (26-28) [58]. In this study, there were four kinds of literature categorized as poor quality, namely Praharsana et al. [59], Nazaruddin & Putri [60], Selivanov & Pobokin [61], and Fadeev et al. [62]. Because of the lack of fair to excellent quality literature, these four literatures were still used as the main source in conducting the literature review.
A total of 6,899 pieces of literature have been found and must still be screened based on inclusion and exclusion criteria. Next, the author will synthesize the research results which involves summarizing the findings of the various selected studies.
3. RESULTS
After going through the screening process according to the stages previously explained, the author succeeded in identifying 8 final articles (Fig. 1). These articles are experimental research using VRET to treat various mental disorders, consisting of 4 articles from Russia and 4 articles from Indonesia (Table 1).
3.1. The Effectiveness of VRET in Treating Mental Disorders Among Early Adulthoods in Russia and Indonesia
In Indonesia, VRET has been proven effective in treating various mental disorders in early adulthood. Research conducted by Fatahillah & Hastarjo showed that VRET is very effective in reducing public speaking anxiety (Fig. 2) [64]. Individuals using VRET can practice in a controlled virtual environment that simulates anxiety triggers, allowing them to confront anxiety-provoking situations without exposure to real-world settings [64]. A study by Nazaruddin & Putri showed that VRET used to be a relaxation tool to relieve general anxiety and has great potential to treat other various anxiety disorders [60]. Users can interact in a calming environment, significantly reducing overall anxiety levels in the environment displayed by VR. Research by Paulus et al. also demonstrated that VRET is effective in reducing fear levels associated with nyctophobia (fear of the dark) by providing users with realistic simulations of dark environments [63]. This gradual exposure allows individuals to confront their fears, helping to decrease the anxiety and fear linked to darkness.
| Articles/Refs. | Participant | Mental Disorder Variable | Country | Results |
|---|---|---|---|---|
| Paulus et al. [63] | 30 undergraduate students, 9 of whom did not complete treatment. 21 participants completed the experiment and were included in the data analysis | Nyctophobia | Indonesia | Research highlights the effectiveness of Mobile-Assisted Virtual Reality in treating specific fears, and it appears that Virtual Reality technology has promising benefits for application to other fears or specific phobias and also use in other psychological treatments. |
| Praharsana et al. [59] | 5 participants: 4 men without spider phobia and 1 woman with spider phobia, aged 20-22 years | Arachnophobia | Indonesia | The VR application succeeded in simulating four spider phobia therapy situations, namely triggering an increase in the user's anxiety level and pulse along with the number of spiders presented, and notably, the single participant with spider phobia showed a significant increase in engagement with the scenarios. |
| Nazaruddin, M.A., & Putri, D.H. [60] | 4 participants aged 19-25 years | Anxiety disorder | Indonesia | Breathing techniques while playing games show that VR has the potential to be a treatment medium for anxiety disorder sufferers, as seen by a decrease in heart rate, feelings of relaxation, motivation to explore and enjoy cosmic wave patterns, and increased focus. |
| Fatahillah, AR., & Hastjarjo. T.D. [64] | Subjects range from 40-50 students aged 18-25 years | Symptoms of social phobia | Indonesia | There was a significant effect of virtual reality exposure on changes in physiological responses and levels of social phobia in students in the treatment group. |
| Selivanov, V.V. [65] | 42 students aged 18-23 years | Anxiety | Russia | Specialized virtual training programs can be used in practice and education to prevent negative emotions in students. The research results show a significant relationship between self-regulation style and anxiety, where the use of immersive VR can reduce anxiety and increase self-regulation, and work programs can be developed. |
| Selivanov et al. [61] | 28 women and 22 men aged 19-25 years | Mental states | Russia | The use of modern helmets in short-term didactic VR programs can cause changes in stable mental state components, such as normal mood, a sense of calm, and significant changes in activation, tone, and euphoria. There is a change in a person's mental state in the VR environment |
| Fadeev et al. [62] | 3 women over 18 years of age | Extreme stress | Russia | Research on three subjects showed that acute emotional stress reactions were elicited by certain VR scenarios. In particular, very strong subjective and autonomic reactions to stressful scenarios associated with fast and uncontrolled movements in VR produce high levels of negative emotional activation in individuals with vestibular disorders and fear of heights. |
| Barabanschikov, V.A., & Selivanov, V.V. [66] | Experimental group of 31 women and 8 men aged 19-24 years, A control group of 12 women and 3 men aged 18-25 years |
Anxiety, depression | Russia | VR technology (specific content) provides a reduction in anxiety levels. VR technology can directly influence the reduction of anxiety levels due to the specific program content. |
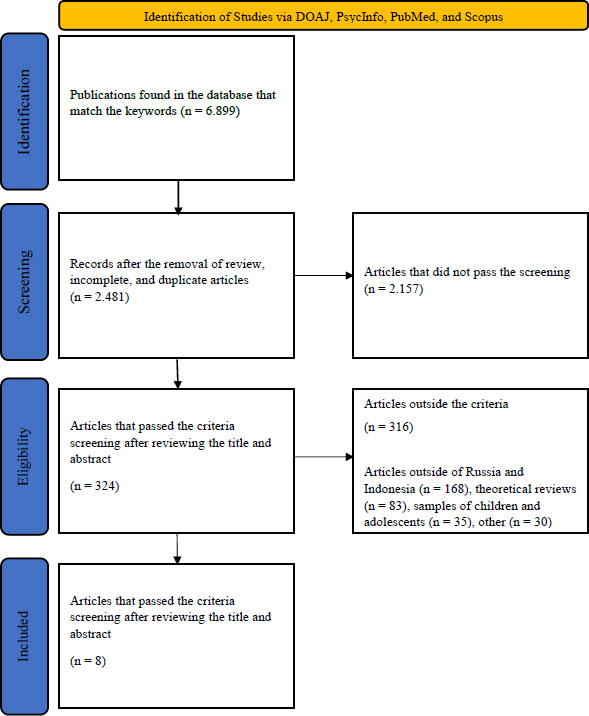
PRISMA flowchart of literature review process.
In Russia, it has also been proven how effective VRET is for the treatment of various kinds of anxiety disorders in early adulthood. The study by Barabanschikov & Selivanov indicated that VRET is effective in reducing both situational and personal anxieties [66]. Furthermore, this form of therapy could also possibly change the behavior of the subconscious mind towards anxiety, which then contributes to the escalation of mood and the reduction of ideomotor symptoms and motor retardations, which are often related to depression [66]. The study by Selivanov and Pobokin also indicated that VRET was effective in alleviating similar anxiety symptoms [61]. This study also showed that VRET enables individuals to develop better-coping strategies towards stress and anxiety. This ability to reduce stress and enhance self-regulation positively impacts individuals’ capacity to cope with various everyday situations [61].
VRET has been proven to be an effective method in Russia and Indonesia, especially in treating anxiety disorders in early adulthood. The effectiveness of VRET conducted in Indonesia is seen in reducing public speaking anxiety, relaxation for general anxiety, and reduced fear of nyctophobia. Meanwhile, in Russia, VRET is effective in reducing situational and personal anxiety and also changing subconscious attitudes towards anxiety.
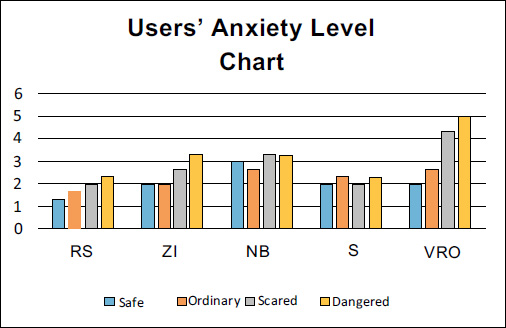
Graph of users’ anxiety level when using VRET as an assessment of the level of fear of spiders in research by Praharsana et al. [59].
3.2. VRET as the Assessment Tool for Mental Conditions Among Young Adults in Russia and Indonesia
In Indonesia, VRET has been used to assess mental disorders in early adulthood, such as arachnophobia (fear of spiders), through various methods. A study by Praharsana et al. [59] demonstrated that evaluation was carried out by observing users’ anxiety responses to a virtual environment featuring spiders. When VRET was conducted, the therapist also installed a heart rate monitor to observe the changes that occurred during the process. Results of the research showed a significant increase in anxiety levels from users with fear of spiders (Fig. 2). User RS showed the lowest anxiety levels across all categories. User ZI experienced moderate anxiety, with a noticeable increase in the “Dangered” category. User NB displayed moderate to high anxiety, especially in the “Scared” and “Dangered” categories. User S had stable and moderate anxiety levels throughout. User VRO showed the highest anxiety across all categories, particularly in the “Scared” and “Dangered” categories. An evaluation was also performed on users’ reactions towards various virtual scenarios, commencing from the least scary to the scariest scenario, in order to obtain a further understanding of the effectiveness of virtual reality therapy [59].
Meanwhile, in Russia, VRET was used to measure mental disorders or conditions in young adults through a physiological and comprehensive response. The study by Fadeev et al. [62] indicated that the assessment involved the measurement of autonomic nervous system activity, EEG (Electroencephalography), heart rate, heart rate variabilities, electrodermal, and respiratory. This study gives a more in-depth picture of how VR could influence various physiological aspects in the response to virtual environment stimuli [62]. Moreover, a study by Selivanov [65] recorded eight different mental conditions to evaluate the participant’s mental activations. The measurements were carried out twice; the first one was after interacting with the VR program, and the second was after the break session. This approach enabled the researchers to understand the shift in mental conditions as the result of VR application and if the effect is sustainable or subsided after the break session. This study also involved control groups that used the same VR program but on a regular monitor to compare the effect between a truly immersive VR and a regular VR [65].
3.3. The Comparisons of the Tools Used in VRET for Treating Mental Disorders Among Early Adults in Russia and Indonesia
In Indonesia, there were several VRET devices that were used for the treatment of anxiety disorders in early adults. Fatahillah & Hastarjo created a realistic virtual environment for exposure therapy by using the VR VIVE HTC device connected to their Windows 10 PC [64]. Meanwhile, Nazaruddin & Putri used the VR Oculus Quest along with controllers, oximeters, and smartphones, which enabled more intense monitoring and interaction throughout the therapy session [60]. The study by Paulus et al. was carried out using a Samsung Gear VR along with wireless headphones, wireless joysticks, and smartphones, creating a higher flexibility and ease of use [63]. On the other hand, Praharsana et al. used the VR Google Cardboard connected to a smartphone and developed the exposure therapy program using Unity software. Besides the simplicity, this device was proven to be effective in giving a realistic exposure therapy experience [59].
In Russia, there were various kinds of VRET devices that were used in the studies, with some studies emphasizing certain technologies. Both studies by Barabanschikov & Selivanov and Selivanov & Pobokin were carried out using the VIVE Helmets, which supported the EMDR (Eye Movement Desensitization and Reprocessing) technique and the Unity software to develop the therapy program [61, 66]. This also shows the popularity of the EMDR technique in the treatment of anxiety disorders in Russia. A study by Fadeev et al. [62] used the HTC VIVE VR HMD device connected to a high-spec PC (Intel Core i7-7700, 16GB RAM, NVIDIA GeForce 1080, and 220GB SSD). With these specifications, the device gave a promising and advanced therapy experience. Meanwhile, Selivanov also used the VIVE Helmets, but without the EMDR approach, and indicated the same effectivity in giving out the therapy required [65].
4. DISCUSSION
The main objective of this research is to analyze the use of Virtual Reality Exposure Therapy (VRET) technology in treating mental disorders among young adults in Russia and Indonesia by reviewing relevant literature. We identify how VRET is applied in the two countries and evaluate its effectiveness and potential in solving the high prevalence of mental disorders in the population of early adulthood in Russia and Indonesia. In our review, we found two important aspects that need to be discussed further. First, the use of VRET as a tool for the assessment of mental disorders, where this technology not only served as therapy but also as a potential mental disorders diagnostic instrument. Secondly, we compare the progress and development of VRET technology between these countries to see how the implementation and adaptation of this technology differs in the two countries.
The use of VRET in Russia and Indonesia is mainly focused on treating anxiety disorders, where it has been shown to be effective. However, VRETs have a high potential to treat other mental disorders besides anxiety disorders, such as personality disorders, Post-Traumatic Stress Disorders (PTSD), attention-deficit/hyperactivity disorder (ADHD), and even severe psychotic disorders. Early conducted research has shown that VRET has been successfully developed to help psychotic patients increase their social participation [67-70].
VRET become a promising intervention to treat various mental disorders in early adulthood. Adverse Childhood Experiences (ACEs) can lead to psychological distress and increase the risk of violent behavior in early adulthood [71, 72]. The transition from adolescence to adulthood is a complex task, often accompanied by stress and individual challenges that commonly happen in college students [73, 74]. As an alternative form of intervention, VRET provides an opportunity for young adults to overcome their problems and develop their resilience in facing the challenges at this stage. It found that VR immersion impacts engagement across all age groups. Therefore, VR can be suitable for individuals aged 18 to 69 years [75].
Although it has been proven to be effective, VRET could also trigger a very common side effect known as cybersickness. Cybersickness in VR is a set of negative symptoms experienced by users during or after VR sessions, similar to motion sickness, due to the immersive nature of VR environments and disconnection between visual input and physical sensations so that the user feels discomfort and disorientation experience [76-81]. Cybersickness could cause symptoms that could not be ignored by both client and therapist, such as headaches or nausea [82]. There is significant variability in how individuals experience and recover from cybersickness. Factors such as individual susceptibility, the type of VR content, and the design of VR systems can influence the severity and duration of symptoms [83, 84]. The level of anxiety plays an important role in cybersickness, especially in triggering the level of nausea, excessive sweating, headache, vestibular discomforts, and oculomotor issues in the user’s experience [85-87, 76]. The research also shows that this nauseous and discomfort feeling could potentially reduce the frequency of use of VR and extensively hinder the acceptance of this technology by individuals.
To mend this problem, therapists are advised to prepare their clients for possible side effects and optimize their VR device settings. A precise set of settings, such as a high refresh rate (120fps or 180fps) and reduced Field of View (FOV), are proven to be effective in reducing simulator sickness without interfering with the user’s experience, increasing the efficacy and satisfaction of the use of VRET [88-91]. This highlights the importance of evaluation and technical optimization in increasing the effectiveness of VRET. If cybersickness has already occurred, it is recommended to take a rest from the virtual environment and engage more in activities that promote recovery, such as resting in a comfortable position, drinking water, and focusing on stable objects in the real world [92, 93].
It was also found that there were several biofeedback tools that could be used by therapists in the VRET therapy sessions, such as EEG (Electroencephalogram), heart rate monitor, respiratory monitor, electrodermal activity, oximeter, and EMDR (Eye Movement Desensitization and Reprocessing). These tools are beneficial as a support in observing and managing the physiological responses during therapy. The use of biofeedback tools is not a novel concept in therapy; for example, an EEG headband was used to observe brain activity during a meditation session [94], and EMDR as a first-line therapy for Post-Traumatic Stress Disorder [95]. Other research also showed that by observing the reduction of brain activity, VRET was effective in reducing the level of anxiety and phobia [96]. The EEG, in particular, could provide valuable insights into the responses of the brain during VRET sessions, which then enriches the understanding of neurological mechanisms behind the therapeutic effects of virtual reality exposure towards anxiety and phobia. With this flexible capability, VRET could be easily integrated with other technologies, such as biofeedback tools, increasing the success of this therapy. Currently, Artificial Intelligence technology that has been widely discovered can also be integrated into VRET and treat various mental disorders which can help the therapist to be more objective [97, 98]. This finding highlights the strong potential of VRET, which continues to evolve, as an accessible solution for addressing the challenges of mental disorders.
It can be seen that the comparison in the use of VRET in Indonesia and Russia shows a notable difference in preferences towards the technologies that were used. In Indonesia, most of the devices that were used were more affordable, such as Oculus Quest, Samsung Gear VR, and Google Cardboard. On the other hand, in Russia, they often used VIVE Helmets that support EMDR and also the Unity Engine software, indicating an integrated and advanced technological system.
The two countries illustrate triumphs in the implementation of these various devices to create an effective therapy for early adults who are experiencing anxiety disorders. The prices and technological advances of the device could directly affect the quality and comfort of the user during therapy sessions. Research showed that the quality of the hardware used in VRET could affect the effectiveness of the therapy [56]. The use of more advanced technology is considered to be important in increasing the VRET results in treating phobic anxiety disorders, including specific phobias [99]. On the other side, the use of low-cost hardware makes these technologies more accessible to individuals with limited resources, allowing for reduced financial barriers and increasing widespread adoption in therapy settings [98, 100].
The companionship and the bilateral collaborations between Russia and Indonesia, especially in mental health care, have a considerable potential to provoke an exchange of scientific knowledge and technological advances. In government policy, digital health transformation in Russia has been a national goal since 2018, while digital health transformation in Indonesia has been a national goal since 2021 [101, 102]. These dynamics could potentially accelerate the development of VRET and improve its accessibility to various sections of society. The rapid technological advances have quickened the recognition of society towards technology, including the virtual reality technology. In Indonesia, the use of VRET is still rare in daily life, including as an entertainment or digital intervention.
On the other hand, challenges like the war conflicts in Russia or the geographic vulnerability of Indonesia towards natural disasters increase the risk of people getting mental health disorders such as depression, anxiety disorders, and even PTSD. Therefore, it is important for both countries to utilize available human resources and technologies to accelerate the development of VRET. This technology has proven effective in treating a variety of mental disorders, allowing individuals to face and overcome their fears in a controlled virtual environment.
5. LIMITATIONS AND CHALLENGES FOR FURTHER RESEARCH
This review is limited by the small number of available and relevant studies analyzed, which restricts the depth and generalizability of the findings. The scarcity of resources poses a significant challenge for future research, particularly in capturing the full potential of VRET as a psychological intervention. Researchers in Indonesia and Russia have approached VRET from various angles within clinical and educational psychology, yet the diversity in research scopes, questions, and variables remains underexplored. Future studies are needed to bridge these gaps and support the evolving needs of psychologists and academics. This is particularly relevant to institutions such as the Faculty of Psychology at Universitas Islam Riau, which has a strategic role in advancing psychological interventions and interdisciplinary research, especially within the context of educational sciences in higher education.
CONCLUSION
The use of Virtual Reality Exposure Therapy (VRET) among young adults in Russia and Indonesia highlights its increasing relevance in the treatment of various mental health disorders, particularly anxiety-related conditions. In Indonesia, VRET is primarily utilized for addressing specific phobias, such as arachnophobia and nyctophobia, as well as social phobia. In contrast, studies in Russia demonstrate a broader application, extending beyond anxiety to include stress management and depression treatment. This suggests that while both countries recognize the value of VRET, they differ in the scope and depth of its implementation.
A notable distinction lies in the integration of physiological monitoring tools. Indonesian research has mainly relied on heart rate as a physiological indicator, whereas Russian studies incorporate more varied and advanced tools, such as electrodermal activity, respiration tracking, and EMDR (Eye Movement Desensitization and Reprocessing). Despite these differences, it is important to emphasize that technological advancement alone does not determine therapeutic success. The therapist's ability to guide clients through the core principles of exposure therapy remains the most crucial factor in achieving positive outcomes with VRET.
For future development, research should explore the potential of VRET in treating a wider range of mental health disorders beyond anxiety. Standardized guidelines and culturally adaptable protocols are essential to support the global implementation of VRET across different languages, regions, and healthcare systems. In addition, experimental studies focusing on more specific phobia types and target populations would help deepen the understanding of VRET’s effectiveness. Mental health institutions in both Russia and Indonesia are also encouraged to support the adoption of accessible, technology-based interventions like VRET, which can offer scalable, cost-effective solutions to meet growing mental health needs.
AUTHORS’ CONTRIBUTIONS
The authors confirm contribution to the paper as follows: B.H., S.F.R.: Study concept or design; A.V.L.: Writing, reviewing and editing; W.I.: Methodology; A.M., I.L.S., D.S.: Collaborator. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| VR | = Virtual Reality |
| VRET | = Virtual Reality Exposure Therapy |
| EEG | = Electroencephalography |
ACKNOWLEDGEMENTS
The authors would like to thank the reviewers for the constructive feedback and all those who have contributed to the making of this article.