All published articles of this journal are available on ScienceDirect.
Psychotic Experiences in Borderline Personality Disorder: The Relationship with Childhood Trauma
Abstract
Introduction
This study aimed to explore the relationship between psychotic experiences, their severity (distress), and childhood trauma in individuals diagnosed with borderline personality disorder (BPD) within an Egyptian adult population.
Methods
Using a cross-sectional design, the study analyzed psychotic experiences, associated distress, and childhood trauma in a sample of 117 participants, including individuals with BPD and matched controls. Standardized self-report measures were administered to assess psychotic experiences, psychotic symptom severity (distress), and childhood trauma history. Path analysis was conducted to investigate trauma types as predictors of psychotic outcomes and BPD diagnosis.
Results
Participants with BPD reported significantly higher levels of psychotic experiences and distress compared to controls. All subtypes of childhood trauma were more prevalent in the BPD group. Among these, physical neglect and sexual abuse emerged as significant predictors of psychotic symptoms and distress. Path analysis identified physical neglect as the strongest predictor of BPD, showing both direct and indirect effects on psychotic symptomatology.
Discussion
The findings highlight the role of specific trauma types - particularly physical neglect - in the development of BPD and its psychotic features. By integrating Linehan’s Biosocial Model with trauma theory, the study emphasizes how early neglect may shape invalidating environments, contributing to BPD symptom expression. Physical neglect appeared to be a key risk factor, potentially contributing to BPD development and subsequent psychotic experiences and distress in Egyptians.
Conclusion
The study expanded existing research on trauma-based models of BPD and its psychotic symptoms, providing culturally relevant insights into the impact of childhood trauma and emphasizing the role of social environments and early relational experiences in non-Western contexts. By integrating Linehan’s Biosocial Model with trauma theory, this study's findings highlighted that early physical neglect – often overlooked in BPD models – may strongly contribute to shaping invalidating environments and thus influencing BPD symptom expression.
1. INTRODUCTION
Borderline personality disorder (BPD) is a complex mental disorder characterized by a general pattern of emotional outbursts, poor management of interpersonal relationships, and an unstable self-image with symptoms that may include fear of abandonment, unstable identity, impulsivity, suicidal ideation, emotional dysregulation, transient paranoid thoughts, and dissociative episodes [1, 2]. Individuals diagnosed with BPD are often stigmatized and viewed as hopeless and resistant to therapy [3]. Such stigma often occurs due to a misunderstanding of the nature and development of BPD [4-6].
Studies suggest that both the development of BPD and its associated psychotic experiences are often linked to past traumatic experiences and childhood trauma, in particular [7-9]. Patients diagnosed with BPD often report experiencing psychotic symptoms, including hallucinations, distorted body images, reference thoughts, paranoid symptoms, and hypnogogic symptoms [9]. The most commonly reported symptoms in BPD are auditory hallucinations, which often echo past traumas [10-15].
While past studies have established a general association between childhood trauma and BPD, there is a significant gap in understanding how specific trauma types may shape the presentation and severity of psychotic symptoms in BPD patients. Moreover, most existing research has focused on Western populations, leaving the influence of sociocultural factors and psychotic symptomatology in non-Western settings largely unexplored. Notably, up to the authors’ knowledge, no prior research has examined the prevalence and characteristics of psychotic symptoms in Egyptian individuals with BPD, nor their relationship to specific childhood trauma types. Addressing this gap is crucial for refining diagnostic frameworks and developing culturally relevant interventions.
To fill in this research gap, this study investigates the relationship between specific childhood traumatic experiences and the presentation and severity of psychotic symptoms in Egyptian adults with BPD. This study provides new insights into trauma-related mechanisms in BPD, supporting the development of culturally informed diagnostic frameworks and interventions tailored to non-Western populations.
1.1. Borderline Personality Disorder and Psychotic Experiences
Psychotic symptoms in BPD can be quite distressing, yet they are frequently overlooked in clinical settings and sometimes labelled as pseudo-psychotic and quasi-psychotic [16, 17]. Recent studies suggest that psychotic symptoms in BPD exist on a continuum, with distressing experiences ranging from pseudo-psychotic episodes and quasi-psychotic manifestations to true psychosis [11, 13]. In this study, psychotic distress is defined as the emotional suffering associated with psychotic-like experiences, such as auditory hallucinations or delusions [18]. While individuals with BPD may not meet the criteria for a full psychotic disorder, they often experience significant distress related to these symptoms, impacting their overall functioning [19]. In this regard, pseudo-psychotic episodes are those similar to true psychosis, yet lacking the severity, persistence, and/or loss of insight observed in the latter. Additionally, quasi-psychosis refers to transient, psychotic-like episodes reactive to emotional distress, which might not fully align with a psychotic disorder. Such quasi-psychotic experiences in BPD often include paranoid ideation, auditory hallucinations, and dissociative states [11, 20].
While psychotic experiences in BPD can be transient, research suggests that certain symptoms may persist and resemble those observed in psychotic disorders [8, 17, 19, 21]. Thus, the hallucinatory experiences in BPD patients were found to be phenomenologically similar to those described in the schizophrenia spectrum in their vividness, duration, and spatial localization [12]. For instance, a study on 171 BPD patients found that 30% experienced persistent and distressing auditory hallucinations [22]. Another study showed that despite the occurrence of stress-related psychotic episodes in BPD patients, they were significantly more likely to experience persistent and reactive hallucinations compared to control groups [23]. It has been reported that the prevalence of positive psychotic symptoms among BPD patients ranges from 13% to 60%, with auditory hallucinations being the most common manifestation [10-15, 24]. One study showed that 50% of BPD patients experienced auditory hallucinations, 30% had visual hallucinations, 20% had delusions, 13% had tactile hallucinations, and 10% had olfactory hallucinations [25].
Beyond prevalence rates, some research highlighted qualitative differences of psychotic experiences in BPD patients, compared to those in other disorders. For instance, it was demonstrated that individuals diagnosed with BPD experienced more guilt-related delusions compared to patients with schizophrenia [13]. Additionally, BPD auditory hallucinations tended to be more self-critical and derogatory [12, 13]. Yet, it is important to emphasize that psychotic symptoms in BPD are still not fully understood, especially those other than auditory hallucinations [10].
1.2. Borderline Personality Disorder and Childhood Trauma
Childhood trauma refers to experiencing or witnessing events that pose a serious risk of death or injury and cause extreme arousal, exceeding one’s capacity to cope, tolerate, or accept it, therefore causing continuing negative consequences on one’s mental health and well-being, including persistent flashbacks, psychosocial and interpersonal difficulties, and psychosomatic symptoms [26]. All forms of childhood trauma experiences are highly prevalent among individuals with BPD, with studies estimating that between 30% and 90% of all BPD patients report some sort of childhood physical or emotional abuse [27]. These adverse experiences, occurring before the age of 18, include sexual abuse, physical abuse, as well as emotional abuse and neglect [26, 28]. Overall, research indicates that BPD is more strongly associated with childhood adverse experiences than any other personality disorder [29]. A study of 358 BPD patients found that 84% had experienced some form of physical, verbal, and emotional childhood abuse and neglect compared to 61% in the control group [30, 31].
Particularly, sexual trauma is frequently reported among BPD patients. For instance, a study conducted on 290 individuals showed that the extent of the experienced childhood sexual abuse contributed to the severity of borderline symptoms [2]. Another study supported these findings by showing that sexual abuse alters self-identity, social status, and self-regulation, contributing to BPD development [32]. However, while sexual abuse acts as a risk factor in the onset of BPD, it is not directly linked to the emotional distress experienced by BPD patients [33, 34].
Studies indicate that adverse childhood experiences contribute to BPD development through shaping attachment styles, with disorganized attachment emerging when a child perceives their caregiver as both a source of comfort and threat due to abuse or neglect [35]. In environments where caregiver responsiveness is inconsistent or absent, children struggle to develop trust, fostering emotional instability and interpersonal difficulties, which are core features of BPD [36, 37]. Finally, Kernberg’s object-relations model explains that identity diffusion, impaired reality testing, and emotional dysregulation - distinctive symptoms of BPD - are caused by disruption in the integration of caregiver-based object relations [26, 38]. This model suggests that early relational trauma shapes negative self-perception and distorted interpersonal expectations, reinforcing core BPD pathology [39].
However, some studies suggest that childhood trauma is not the primary factor in BPD development. A systematic review of 19 longitudinal studies did not support the link between childhood maltreatment and BPD diagnosis. The review found that the relationship was stronger in studies relying on a symptom count rather than a categorical diagnosis of BPD [40]. Additionally, a twin study examining the association between childhood trauma and BPD found little to no evidence of a causal relationship between the two variables, instead citing that the associations are a result of shared genetic influences [41]. These findings highlight the need for more research to clarify the link between childhood trauma and BPD.
Some studies emphasizes the role of the hypothalamic-pituitary-adrenal (HPA) axis in mediating structural changes resulting from childhood trauma, which potentially contributes to dissociation and BPD-related psychosis [42]. Persistent activation of the HPA axis prolongs the impact of childhood traumatic experiences by maintaining a heightened state of alertness, leading to hyperactivity of the stress response system [12, 43-46]. HPA axis dysfunction has been linked to overthinking, anxiety, and depression in BPD individuals [47], with early adversities potentially predisposing individuals to dysregulation and to BPD development [44]. Heightened emotional arousal and stress cause misinterpretation of internal thoughts or memories as external stimuli, leading to hallucinations and other psychotic symptoms in individuals with BPD [9, 15, 16, 48-52]. Due to the influence of past trauma, these hallucinations often carry a negative tone, mirroring the previously experienced abuse or neglect [12, 25]. While the HPA-BPD psychosis link remains an emerging theoretical framework, neurobiological research suggests that chronic stress-reactive dysregulation due to early trauma may contribute to stress-induced psychotic symptoms [41].
Trauma during critical periods of development was linked to maladaptive coping mechanisms and emotional regulation skills, with dissociation mediating the relationship between childhood trauma and psychotic symptoms in BPD [16, 53]. Furthermore, the prevalence of psychotic symptoms among individuals with BPD who have experienced trauma highlights the profound and lasting impact of early adverse experiences on mental health [12, 25]. Specifically, auditory hallucinations have been frequently reported as negative and distressing, deeply rooted in the individual's past traumatic experiences. For instance, individuals with BPD who experienced verbal abuse during childhood may ‘hear’ accusatory or threatening voices, echoing language used by their abusers [53, 54]. These distressing hallucinations may reinforce the individual's feelings of worthlessness, heightened anxiety, mistrust, paranoia, and fear [16]. Studies showed that these hallucinations were not arbitrary; instead, they often reflected the emotional and psychological scars left by childhood trauma [9, 55].
The strong connection between childhood trauma and psychotic symptoms in BPD highlights the complex interplay between early life experiences, biological vulnerability, and psychological manifestations. This interaction aligns with emerging trauma theory, which emphasizes how early adversity disrupts neurodevelopment and stress regulation, increasing susceptibility to emotional dysregulation and psychotic distress [46]. Additionally, this supports Linehan’s Biosocial Model of BPD development, suggesting that neurobiological vulnerabilities interact with psychosocial risk factors, such as childhood trauma and invalidation, to shape BPD symptom expression [56]. The integration of trauma theory and the biosocial model provides a comprehensive framework for understanding how early adversity contributes to both emotional dysregulation and psychotic distress in BPD in our study.
Within Linehan’s Biosocial Theory, BPD is a disorder of emotion dysregulation, shaped by both biological predispositions and environmental influences [56]. Individuals with BPD have an innate emotional vulnerability, characterized by intense emotional reactions and difficulty returning to baseline after distressing events [56, 57]. When this biological predisposition interacts with an invalidating environment, such as childhood trauma, maladaptive emotional and cognitive patterns are reinforced, contributing to BPD development [56, 58]. If an individual’s emotional responses are dismissed, punished, or ignored due to neglect, emotional abuse, and physical maltreatment, an invalidating environment is formed, leading to chronic emotional instability and identity disturbances [56, 58].
Research has also found that neglect and emotional abuse are among the strongest predictors of psychotic experiences in BPD, reinforcing the biosocial model’s emphasis on environmental invalidation as a key factor in symptom development [58]. This transactional model also explains why individuals with BPD often experience a continuum of psychotic symptoms, since they may emerge as maladaptive coping mechanisms in response to early invalidation and trauma [56].
1.3. Differential Impact of Childhood Trauma on BPD and Psychotic Symptoms
Emerging research has examined the relationship between specific types of childhood trauma, including physical and emotional abuse, sexual abuse, emotional neglect, and physical neglect, and BPD [30, 59-64]. Despite wide recognition of childhood trauma as a major risk factor for the development of BPD, the differential impact of trauma types remains unclear.
Some studies reported a higher association between BPD and emotional neglect and emotional abuse [65]. In particular, emotional neglect – through deprivation of validation and emotional support – was shown to enable chronic feelings of emptiness and interpersonal hypersensitivity in individuals with BPD, further reinforcing the disorder’s core symptoms [35]. One study found that emotional abuse was the only significant predictor of BPD and only in men [66].
Other research suggested a strong relationship between sexual and physical abuse and severe emotional neglect [7]. Furthermore, physical and sexual abuse were most frequently linked to psychotic experiences and overall clinical presentation of BPD, particularly in women [52, 67, 68]. Sexual assault was specifically linked to hallucinations [69, 70]. However, it is important to note that many studies have a priori explored the link between sexual and physical abuse and BPD, excluding other trauma types from the analysis, which might have influenced the findings. More recent meta-analyses of childhood adversity and BPD reported more negative associations between sexual abuse and BPD [29]. Conversely, physical neglect was found as the most common form of childhood trauma among BPD participants (48.9%) [29]. Among other strong predictors of psychotic experiences in BPD were emotional abuse associated with schizotypal symptoms [7].
Understanding the differential impact of childhood trauma types on BPD and psychotic symptoms is essential for developing targeted interventions. However, the limited number of studies conducted in non-Western contexts, as well as the lack of consensus regarding differential effects of childhood adversity due to the frequent co-occurrence of childhood trauma types in BPD individuals, makes it challenging to isolate specific effects of each type on BPD development and symptomology. Thus, further research is needed, particularly in cross-cultural settings, to examine how childhood trauma may uniquely shape BPD presentation in diverse populations.
Based on prior research and the conceptual framework outlined above, our study will test the following hypotheses: (H1) different types of childhood trauma will be reported more frequently among BPD individuals compared to the control group, and (H2) different types of childhood trauma will have distinct effects on psychotic experiences and psychotic distress in individuals with BPD.
2. METHODOLOGY
2.1. Design
This quantitative research utilized a descriptive cross-sectional correlational design to identify the degree of relationship between borderline personality disorder, the presence and severity of psychotic experiences, and childhood trauma among adult Egyptians. The quantitative study's aim was to shed light on the relationships between these variables, with a special focus on the impact of kinds of childhood trauma on the presentation and severity of psychotic symptoms in BPD Egyptian adults.
2.2. Participants
The study employed both purposeful, convenience, and snowball sampling methods to recruit participants. The questionnaires were disseminated online, targeting both the general public and individuals diagnosed with borderline personality disorder (BPD) who were readily available. By using these sampling techniques, the study aimed to gather a diverse and representative sample of Egyptian adults to explore the relationships between the variables under investigation.
The target participants of the study were Egyptian adults aged 18 to 40, both diagnosed with BPD and self-identifying as having no mental health impairment. Individuals diagnosed with any form of cognitive impairment or condition that would affect cognitive function were excluded from this study to ensure the reliability and validity of the results. All participants included were required to have typical cognitive function, as self-reported. Participants were recruited from diverse backgrounds to ensure diversity in experiences and relevance to the age range of BPD.
2.3. Assessment Tools
First, the shortened version of the Borderline Symptom List (BSL-23), a 23-item patient self-reported scale, was used to screen for the borderline personality disorder symptomatology. It was derived from the longer BSL-95, which aims at assessing the severity classification of DSM-5 aligned symptoms of BPD in individuals aged from 18 y.o [71]. The BPD-23 scale items assess the following symptoms and cover the following diagnostic criteria: affective instability about an individual`s character or could encompass features of ‘anger’, ‘depression’ or ‘anxiety’ (i.e., as the 14th item highlights: ‘My mood rapidly cycled in terms of anxiety, anger, and depression’), recurrent suicidal behavior, threats, gestures or self-mutilating behaviors (i.e., ‘I didn’t believe in my right to live’, ‘The idea of death had a certain fascination for me’, ‘I thought of hurting myself’, ‘I wanted to punish myself’), transient dissociative phenomena (i.e., ‘I felt as if I was far away from myself’), ‘self-criticizing’ behavior (i.e., ‘Criticism had a devastating effect on me’), trust related issues (i.e., ‘I didn’t trust other people’), involuntary emotional aspects of vulnerability and ‘shame’, a ‘self-hate’ feeling, a feeling of being ‘alone’ sensation, and ‘helplessness’ feeling of being ignored’ [71].
The 21-item Prodromal Questionnaire, Brief Version (PQ-B) was used for psychosis risk screening. It is a 21-item shortened version of the 92-item Prodromal Questionnaire [18]. The 21-item PQB is a self-report questionnaire, consisting of positive symptoms questions and additional questions related to the severity of these symptoms, or distress caused by these symptoms and their functional effects. The PQ-B measures two key constructs related to psychosis, including psychotic experiences and psychotic distress. Psychotic experiences (PE) refer to hallucinations, delusions, or perceptual distortions that signal prodromal (early) psychosis, which ranges from mild and transient to persistent and distressing. Meanwhile, psychotic distress is defined as the emotional suffering caused by such psychotic symptoms. The distress can manifest as anxiety, fear, confusion, or impairment in daily functioning.
The PQ-B includes yes/no questions about psychotic-like experiences, followed by distress ratings for each endorsed symptom. Example PE items include, ‘Do you ever hear things that other people do not hear?’ or ‘Do you ever feel that your thoughts are being controlled by outside forces?’. Symptom endorsement is coded as No = 0, Yes = 1, with endorsed symptoms assessed using a Likert scale for distress (1 = ‘strongly disagree’, 2 = ‘disagree’, 3 = ‘neutral’, 4 = ‘agree’, and 5 = ‘strongly agree’). A Distress Score ≥ 6 is often used as a cutoff for identifying individuals at higher risk for psychosis [18]. The maximum possible psychotic experiences score is 21, while the maximum possible score of psychotic distress is 105. All the versions of the PQ appeared to be accurate in identifying individuals with ultra-high risk syndrome for psychosis with different thresholds [72].
The 28-item Childhood Trauma Questionnaire–Short Form (CTQ), adapted from the original 70-item questionnaire, was used to assess adverse childhood experiences of the participants. This self-report questionnaire encompasses different kinds of abuse and trauma, including emotional abuse, physical abuse, sexual abuse, physical neglect, and emotional neglect that occurred during childhood and adolescence, up to the age of 18. This structured retrospective self-report tool has been proven reliable and valid for assessing a broad range of traumatic experiences in childhood. The five scales included the following. Emotional Abuse (EA) refers to verbal assaults, criticism, or demeaning behavior that affects a child's sense of self-worth (i.e., ‘People in my family called me things like ‘stupid,’ ‘lazy,’ or ‘ugly.’). Physical Abuse (PA) involves bodily harm or injury inflicted through hitting, slapping, or other forms of physical aggression (i.e., ‘I got hit so hard by someone in my family that I had to see a doctor or go to the hospital.’). Sexual Abuse (SA) refers to an inappropriate sexual contact/conduct towards a child (i.e., ‘Someone tried to touch me in a sexual way, or tried to make me touch them.’). Emotional Neglect (EN) refers to the failure to meet a child's emotional needs for love and support (i.e., a reversed scored statement: ‘There was someone in my family who helped me feel that I was important or special.’). Physical Neglect (PN) describes the lack of provision for basic physical needs such as food, shelter, and medical care (i.e., ‘My family and I did not have enough to eat.’) [73, 74].
2.4. Procedure
Ethical approval for this study was obtained from the Faculty of Arts and Humanities (FOAH) Ethics Committee, British University in Egypt (BUE), prior to data collection. The study data were gathered through an online, self-administered survey conducted via Google Forms, which consisted of three sections. First, participants' informed consent was obtained by directing them to a consent form link, where they were asked to confirm that they had read, understood, and agreed to participate in the study with Yes/No questions. Second, information regarding participants' demographics and backgrounds was collected, including age, self-identified gender, and level of education. Additionally, medical data were gathered, including whether participants had been diagnosed by a psychiatrist or psychologist with borderline personality disorder, the presence of comorbid mental disorders, medications, and drug use.
All participants provided informed consent prior to data collection, in line with institutional and established ethical standards. As no personal or identifiable information was collected or published, specific consent for publication was not required. Data were anonymized and presented in aggregate, ensuring participant confidentiality.
2.5. Data Analysis
To examine the relationships and mediating effects among the study variables, the data obtained were analyzed using several statistical software packages, including IBM SPSS Statistics 23, Jamovi, and JASP. The analytical methods in this study were comprehensive and included t-tests, Generalized Linear Model (GLM) mediation analysis, automatic linear modeling, Bayesian linear regression analysis, and AMOS path modeling. Additionally, the study instruments’ reliability was checked with internal consistency analyses. By using these diverse analytical techniques, the study aimed to provide a robust understanding of the complex interactions and mediating effects present among the variables.
| - | Control Group | BPD Group | ||||||
|---|---|---|---|---|---|---|---|---|
| N | % | SE | SD | N | % | SE | SD | |
| Gender | - | - | 0.049 | 0.398 | - | - | 0.063 | 0.443 |
| Males | 13 | 19.4 | - | - | 13 | 26 | - | - |
| Females | 54 | 80.6 | - | - | 37 | 74 | - | - |
| - | Control Group | BPD Group | ||||||
| N | Mean | Median | SD | N | Mean | Median | SD | |
| Age | 67 | 23.0 | 21.0 | 5.66 | 50 | 24.9 | 23.0 | 6.44 |
| Variables | t | df | p-value | VS-MPR* | Mean Difference | SE Difference | Hedges' g |
|---|---|---|---|---|---|---|---|
| BPD | -4.925 | 105.668 | < 0.001 | 9275.042 | -19.343 | 3.927 | -0.917 |
| Psychotic experiences | -5.384 | 110.144 | < 0.001 | 60235.790 | -4.659 | 0.865 | -0.996 |
| Psychotic distress | -6.517 | 103.390 | < 0.001 | 6.992×10+6 | -24.292 | 3.728 | -1.217 |
| Emotional abuse | -5.797 | 112.179 | < 0.001 | 351984.018 | -5.116 | 0.882 | -1.068 |
| Physical abuse | -5.022 | 93.632 | < 0.001 | 11677.966 | -5.156 | 1.027 | -0.948 |
| Sexual abuse | -3.759 | 82.197 | < 0.001 | 143.486 | -4.201 | 1.118 | -0.717 |
| Emotional neglect | -5.912 | 112.733 | < 0.001 | 583674.192 | -5.050 | 0.854 | -1.088 |
| Physical neglect | -3.778 | 103.685 | < 0.001 | 169.057 | -2.210 | 0.585 | -0.705 |
3. RESULTS
3.1. Descriptive Statistics
Our study sample consisted of 117 adult Egyptians (N=117), aged 18 to 40 (M = 23.8, SD = 6.05). The sample included 91 self-identified females (77,8%), and 26 self-identified males (22.2%). The sample groups’ description is presented in Table 1.
3.2. Scales Reliability Analysis
The reliability of the Borderline Personality Disorder (BPD) scale (23 items) for our study sample was assessed using Cronbach's Alpha, yielding a high reliability coefficient of α=0.950 and a mean item-total correlation of α=0.618. The reliability of the PQ (psychotic experiences) scale was assessed using Cronbach's Alpha, showing a high reliability coefficient of α=0.870 and moderate inter-item consistency of α=487 across 21 items. Finally, the reliability of the Childhood Trauma Scale was assessed using Cronbach's Alpha, yielding α=0.868 across 28 items, indicating its high reliability. The mean inter-item correlation for the scale was α=0.487, reflecting a moderate level of internal consistency.
3.3. Independent Samples t-test
Independent samples t-tests were conducted to compare seven study variables, including BPD screening score, psychotic experiences, psychotic distress, emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect, between the control and BPD-diagnosed groups. Welch’s test was used to determine statistically significant differences between the two groups (Table 2).
Thus, for the borderline personality disorder screening, the Welch’s t-test showed a significant difference between groups, t(105.668)=−4.925t(105.668) = -4.925, p < 0.001, with a mean difference of -19.343 (SE = 3.927), 95% CI [-27.12, -11.56], and a large effect size (Hedges' g = -0.917), indicating that indeed there was a statistically significant difference between the control and study groups. For the psychotic experience, the Welch’s t-test was significant, t(110.144)=−5.384t(110.144) = -5.384, p < 0.001, with a mean difference of -4.659 (SE = 0.865), 95% CI [-6.37, -2.94], and a large effect size of -0.996. This implied that the BPD group participants experienced significantly more psychotic symptoms than those in the control group. The severity of psychotic symptoms was also significantly higher in the BPD group compared to the control group: t(103.390)=-6.517t(103.390) = -6.517, p < 0.001, with a mean difference of -4.292 (SE = 3.728), 95% CI [-31.68, -16.90], and a very large effect size of Hedges' g = -1.217. Similar significant differences were also observed between the two groups in their adverse childhood events experiences. Thus, for physical neglect, the Welch’s t-test indicated a significant difference, t(103.685)= -3.778t(103.685) = -3.778, p < 0.001, with a mean difference of -2.210 (SE = 0.585), 95% CI [-3.37, -1.05], and a medium effect size of -0.705; for emotional neglect, t(112.733)=-5.912t(112.733) = -5.912, p < 0.001, with a mean difference of -5.050 (SE = 0.854), 95% CI [-6.78, -3.32], and a large effect size of Hedges' g -1.088. For sexual abuse, the Welch’s t-test showed a significant difference, t(82.197)=−3.759t(82.197) = -3.759, p < 0.001, with a mean difference of -4.201 (SE = 1.118), 95% CI [-6.42, -1.98], and a medium effect size of Hedges' g = -0.717; for physical abuse, t(93.632) = −5.022t(93.632) = -5.022, p < 0.001, with a mean difference of -5.156 (SE = 1.027), 95% CI [-7.19, -3.12], and a large effect size of Hedges' g =-0.948. For emotional abuse, the Welch’s t-test revealed a significant difference, t(112.179)=-5.797t(112.179) = -5.797, p < 0.001, with a mean difference of -5.116 (SE = 0.882), 95% CI [-6.90, -3.33], and a large effect size of Hedges' g =-1.068 (Fig. 1).
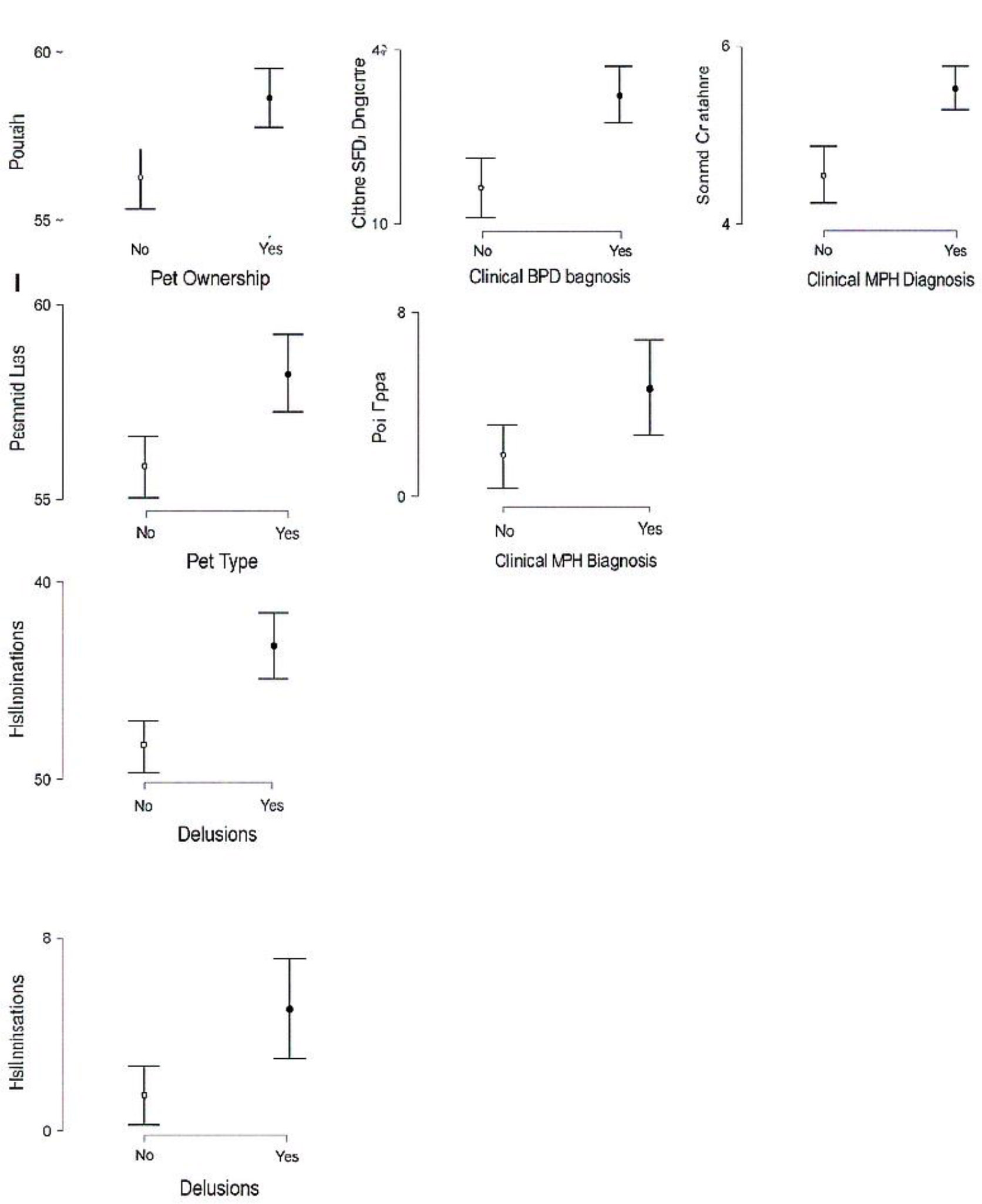
Descriptives plots.
| - | N | Mean | Std. Error | Std. Deviation |
|---|---|---|---|---|
| Emotional neglect | 66 | 12,5303 | 0,61459 | 4,99298 |
| Emotional abuse | 66 | 12,4242 | 0,62841 | 5,10523 |
| Physical abuse | 66 | 9,4242 | 0,59800 | 4,85818 |
| Sexual abuse | 66 | 8,3788 | 0,57239 | 4,65011 |
| Physical neglect | 66 | 7,9697 | 0,37644 | 3,05825 |
| - | N | Mean | Std. Error | Std. Deviation |
|---|---|---|---|---|
| Emotional neglect | 50 | 17,5800 | 0,59322 | 4,19470 |
| Emotional abuse | 50 | 17,5400 | 0,61955 | 4,38090 |
| Physical abuse | 50 | 14,5800 | 0,83451 | 5,90085 |
| Sexual abuse | 50 | 12,5800 | 0,96006 | 6,78862 |
| Physical neglect | 50 | 10,1800 | 0,44784 | 3,16673 |
Levene’s test for homogeneity of variances showed that most variables met the assumption of equal variances, except for Sexual Abuse, which violated this assumption (F(1,114)=14.6492F 1, 114) = 14.6492, p < 0.001).
Regarding the most prevalent adverse childhood experiences in the control group and BPD study group in our sample, individuals in the BPD group reported higher mean scores for all types of adverse childhood events compared to those in the control group. In both groups, the most prevalent kinds of adverse childhood events were emotional neglect and emotional abuse (Tables 3 and 4).
3.4. Automatic Linear Modelling
Next, the automatic linear modelling was run to investigate the relationship between both psychotic experiences and psychotic distress and all the other independent variables in the study, given that the LINEAR analysis gives rather robust results [75]. First, the standard model was built, eliciting four most important predictors of psychotic experiences and psychotic distress: BPD, physical neglect, age, and sexual abuse (Figs. 2 and 3).
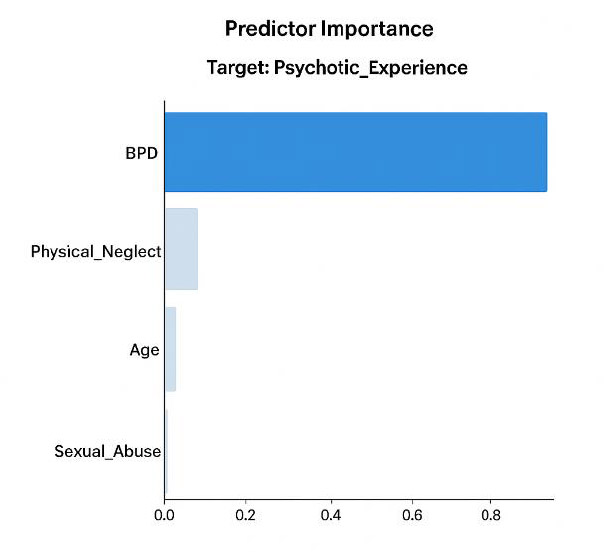
Model predictors for psychotic experiences.
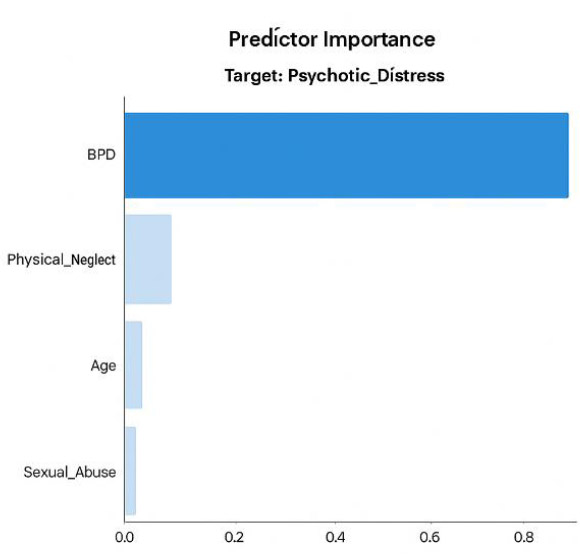
Model predictors for psychotic distress.
The model-building method was forward stepwise using the information criterion.
3.5. Bayesian Linear Regression Analysis
A Bayesian linear regression analysis was then conducted to examine the relationship between the determined variables of age, physical neglect, sexual abuse, and borderline personality disorder (BPD) and (1) psychotic experiences and (2) psychotics distress. Model comparison using Bayes Factors (BF) indicated that the model including physical neglect, sexual abuse, age, and BPD as predictors provided the best fit to the data (BFM = 10.728) to predict psychotic experiences. It also had the highest posterior probability (P(M|data) = 0.728, R2 = 0.581). Similar results were yielded for the dependent variable of psychotic distress. Thus, model comparison using Bayes Factors (BF) indicated that the model including physical neglect, sexual abuse, age, and BPD as predictors provided the best fit to the data (BFM(10) = 6.893) to predict psychotic distress. It also had the highest posterior probability (P(M|data) = 0.633, R2 = 0.623). The analysis of individual predictive relationships between the above independent variables and both psychotic experiences and psychotic distress had a similar pattern. In particular, for both dependent variables, physical neglect had a high inclusion probability (P(incl|data) = 0.969 for psychotic experiences and P(incl|data) = 0.981 for psychotic distress). A positive mean coefficient (M = 0.271 and credible interval 0.000-0.465) indicated that higher levels of perception of childhood physical neglect were associated with an increase in psychotic experiences. Similarly, a positive mean coefficient (1.263 and credible interval 0.323–2.225) indicates a strong association of childhood physical neglect with an increase in psychotic distress. Sexual abuse showed a moderate inclusion probability (P(incl|data) = 0.809) and a positive mean coefficient (M = 0.074), indicating its potential positive relationship with psychotic experiences. However, the credible interval between -0.022 and 0.203 included zero, which suggested some uncertainty. Similarly, for psychotic distress, sexual abuse had a moderate inclusion probability (P(incl|data) = 0.768) and a moderate mean coefficient M=0.281, indicating a positive association with the former. However, the credible interval between -0.058 and 0.834 included zero, which suggested again some uncertainty. Age had a moderate inclusion probability for both psychotic experiences (P(incl|data) = 0.892) with a negative mean coefficient M = -0.092 and for psychotic distress (P(incl|data) = 0.779) with a negative coefficient M = -0.258), implying that younger individuals had more intense psychotic experiences and distress. For both psychotic experiences and psychotic distress, inclusion of age in the model yielded some uncertainty due to the presence of zero in the credible intervals (-0.197 – 0.000 and -0.722 – 0.049 respectively). Finally, BPD had the highest inclusion probability for psychotic experiences (P(incl|data) = 1.000; M = 0.142; the credible interval of 0.108 – 0.170) and psychotic distress (P(incl|data) = 1.000; M = 672; the credible interval of 0.547 – 0.806), indicating a strong and consistent influence of the former on psychotic experiences and psychotic distress (Tables 5 and 6).
| Coefficient | P(incl) | P(excl) | P(incl|data) | P(excl|data) | BFinclusion |
|---|---|---|---|---|---|
| Intercept | 1.000 | 1.000 | 1.000 | 0.000 | 1.000 |
| Physical neglect | 0.500 | 0.969 | 0.969 | 0.031 | 31.126 |
| Sexual abuse | 0.500 | 0.809 | 0.809 | 0.191 | 4.227 |
| Age | 0.500 | 0.892 | 0.892 | 0.108 | 8.221 |
| BPD | 0.500 | 1.000 | 1.000 | 9.437×10-15 | 1.057×10+14 |
| Coefficient | P(incl) | P(excl) | P(incl|data) | P(excl|data) | BFinclusion |
|---|---|---|---|---|---|
| Intercept | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 |
| Physical neglect | 0.500 | 0.500 | 0.981 | 0.019 | 50.544 |
| Sexual abuse | 0.500 | 0.500 | 0.768 | 0.232 | 3.313 |
| Age | 0.500 | 0.500 | 0.779 | 0.221 | 3.535 |
| BPD | 0.500 | 0.500 | 1.000 | 0.000 | 4.573×10+16 |
Overall, both models suggested that physical neglect, sexual abuse, age, and BPD were important predictors of both psychotic experiences and psychotic distress, with BPD being the most crucial factor for both dependent variables.
3.6. AMOS Path Modelling and Mediation Analysis
The best-fitting models identified using Bayesian regression analysis were then verified with Amos path analysis. However, inclusion of only BPD and physical neglect as predictors of both psychotic experiences and psychotic distress yielded the best model fit.
Thus, the AMOS model fit predicting psychotic experiences had an excellent fit to the data. The chi-square value for the default model was 0.000 with zero degrees of freedom, resulting in a CMIN/DF ratio of 0.000. Baseline comparisons further supported the model's fit, with NFI, RFI, IFI, TLI, and CFI equaling 1.000. Parsimony-adjusted measures (PRATIO, PNFI, PCFI) for the default model were also 0.000.
Path analysis results showed that physical neglect significantly predicted BPD (Estimate = 2.131, SE = 0.619, C.R. = 3.442, p < 0.001), and in its turn, BPD significantly predicted psychotic experiences (Estimate = 0.153, SE = 0.015, C.R. = 10.405, p < 0.001). Physical neglect also had a direct significant effect on psychotic experiences (Estimate = 0.284, SE = 0.103, C.R. = 2.760, p = 0.006).
The means for physical neglect were significant (Estimate = 8.897, SE = 0.303, C.R. = 29.357, p < 0.001). The intercepts for BPD (Estimate = 26.388, SE = 5.869, C.R. = 4.496, p < 0.001) and psychotic experiences (Estimate = 2.074, SE = 1.005, C.R. = 2.063, p = 0.039) were also significant. The variances for physical neglect (Estimate = 10.656, SE = 1.399, C.R. = 7.616, p < 0.001), error term 1 (e1: Estimate = 474.080, SE = 62.248, C.R. = 7.616, p < 0.001), and error term 2 (e2: Estimate = 11.843, SE = 1.555, C.R. = 7.616,p < 0.001) were significant (Fig. 4).
Overall, the model fit indices, regression weights, means, intercepts, and variances suggested that the proposed model fit the data well, providing strong support for the hypothesized relationships.
We verified the mediation effect of BPD in the relationship between physical neglect and psychotic experience using the GLM generalized mediation model. The mediation analysis confirmed a significant indirect effect of physical neglect on psychotic experiences through BPD, with an indirect effect estimate of β = 0.205, SE = 0.0992, 95% CI [0.1311, 0.520], z = 3.28, p=0.001. The direct effect of physical neglect on the psychotic experiences was also significant (β = 0.179, SE=0.1023, 95% CI [0.0830, 0.484], z=2.77, p=0.006). The total effect of physical neglect on the psychotic experiences was significant (β=0.384 = 0.384, SE=0.1361, 95% CI [0.3422, 0.876], z = 4.47, p<0.001). For the component pathways, the effect of physical neglect on BPD was significant (β=0.304, SE=0.6166, 95% CI [0.9227, 3.340], z=3.46, p<0.001), as well as the effect of BPD on the psychotic experiences was also significant (β=0.674, SE=0.0146, 95% CI [0.1241, 0.181], z=10.45, p<0.001).
The confidence intervals for these effects were computed using the standard (Delta method).
In contrast, the AMOS path model for the dependent variable of psychotic distress was only marginally fit for our study data. The model fit was evaluated using several indices: for the default model, the chi-square value (χ2(2)=21.736, p=0.000) with a chi-square to degrees of freedom ratio (χ2/df) of 10.868, showed a poor fit.
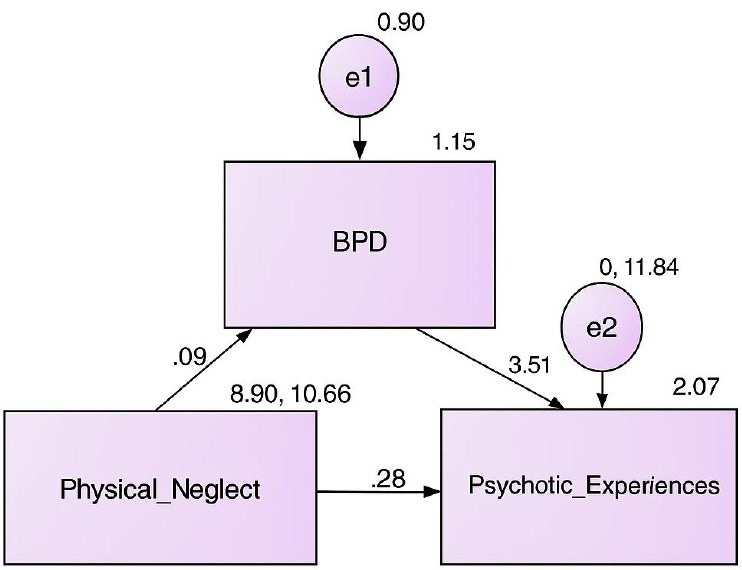
Path model for psychotic experiences.
The independence model's chi-square χ2(10)=146.150, p<0.001), with a χ2/df = 14.615, showed a very poor fit. Baseline comparisons yielded a NFI = 0.851, RFI = 0.256, IFI = 0.863, TLI = 0.275, and CFI = 0.855, which suggested that although the default model fit better than the independence model, the fit was poor. Parsimony-adjusted measures, including PRATIO = 0.200, PNFI = 0.170, and PCFI = 0.171, showed that the model did not balance parsimony, thus fitting poorly. Thus, due to the poor model fit, only the model for psychotic experiences was retained. The differences in the model fits obtained for psychotic experiences and psychotic distress may be explained by a more objective measure of psychotic experiences. Since they have more distinct and measurable symptoms, this leads to a better fit in the AMOS path model. In contrast, psychotic distress is more subjective, often involving emotional and psychological responses to these experiences, which could be influenced by a variety of factors. Besides, psychotic distress may not always correlate directly with the frequency of psychotic experiences, also leading to a poorer fit in the model. However, further mediation analysis was conducted to examine if there were similar indirect effects of physical neglect on psychotic distress through BPD as in the case of the dependent variable of psychotic experiences. The indirect effect of physical neglect on psychotic distress through BPD was found significant, β=0.214, z=3.31, p<0.001, with an estimate of 1.508 (SE = 0.4555), 95% CI [0.616, 2.401]. The direct effect of physical neglect on psychotic distress was also significant, β=0.189, z=3.12, p=0.002, with an estimate of 1.336 (SE = 0.4285), 95% CI [0.496, 2.176]. The total effect of physical neglect on psychotic experience distress was significant, β=0.403, z=4.74, p<0.001, with an estimate of 2.844 (SE = 0.6001), 95% CI [1.668, 4.020]. Component pathways indicated that physical neglect significantly predicted BPD, β=0.304, z=3.46, p<0.001, with an estimate of 2.131 (SE = 0.6166), 95% CI [0.923, 3.340]. BPD significantly predicted psychotic distress, β=0.702, z=11.57, p<0.001, with an estimate of 0.708 (SE = 0.0612), 95% CI [0.588, 0.828]. The confidence intervals were computed using the standard (Delta) method. Hence, the GLM mediation results also suggested that BPD partially mediated the relationship between physical neglect and psychotic distress.
4. DISCUSSION
The purpose of this study was to investigate the relationship between psychotic experiences and childhood trauma among individuals with BPD. Our findings provide compelling evidence to support strong associations between these variables. The findings revealed a significant difference in BPD screening scores between controls and the BPD group, with the latter showing significantly higher scores. which confirmed the validity of our sample selection and group categorization in our study.
In our study, participants clinically diagnosed with BPD reported significantly more psychotic experiences and higher perceived severity of psychotic distress, implying a link between BPD and psychotic symptoms. Findings revealed that emotional neglect and emotional abuse are the most reported forms of childhood trauma among Egyptian adults, in both control and BPD-diagnosed groups. However, further analysis showed that individuals in the BPD group reported higher mean scores for all types of childhood trauma compared to those in the control group. The very large and marginally large effect sizes obtained in the study suggest not only the statistical significance of the results but also their practical significance, implying that the presence of BPD in individuals might be strongly associated with psychotic symptoms and childhood trauma. This finding aligns with the trauma theory and previous research that has consistently demonstrated a strong association between childhood trauma and the development of BPD, emphasizing the critical role of traumatic experiences in the etiology of this disorder [46, 61, 76, 77].
Findings identified four significant predictors of psychotic experiences and severity: BPD, physical neglect, sexual abuse, and age. Subsequently, these predictors were consistent in their influence across both psychotic experiences and psychotic distress, confirming the previous research [78]. Moreover, findings revealed that BPD is the strongest predictor of the presence and severity of psychotic symptoms in individuals. This finding is consistent with previous research on the prevalence of psychotic-like symptoms in individuals with BPD (e.g., visual and auditory hallucinations, paranoia, transient psychotic episodes, and delusions). Another predictor revealed was the age of the study participants, which was negatively linked to the psychotic experience. This finding confirms existing research that younger individuals have higher levels of psychotic experiences [79].
Physical neglect appeared as a significant predictor for both psychotic experiences and psychotic distress. This suggests that childhood physical neglect contributes to increased psychotic symptoms. In addition, sexual abuse showed a moderate inclusion probability for psychotic experiences and psychotic distress. This finding is consistent with studies suggesting that childhood sexual abuse is a significant risk factor for developing BPD [80], and psychotic experiences of abnormal perception [81]. Thus, younger individuals diagnosed with BPD and having experienced a traumatic childhood trauma of physical neglect and/or sexual abuse would experience more frequent and more severe psychotic symptoms compared to other people.
Furthermore, the findings revealed a significant positive direct effect of physical neglect on psychotic experiences, as well as an indirect effect mediated by BPD. Thus, physical neglect significantly predicted BPD, which in turn significantly predicted psychotic experiences. This interesting finding of our study was in line with growing yet scarce research on the effect of physical neglect on psychotic presentation in general and in BPD individuals in particular. Physical neglect was found to be the key predictor of psychotic symptoms and distress. This might be explained with the findings by Schreier et al. [82] that only childhood physical neglect experiences (like having to wear dirty clothes, etc.), but not other forms of childhood trauma measured with CTQ, were related to the exaggerated inflammatory responses to stress and subsequent changes in gene expression. This also aligns with the postulate of the core role of invalidating environment in BDP development in Linehan’s Biosocial Theory. Usually, researchers elicit four characteristics of invalidating environments, including communication of inaccuracy, misattribution, discouragement of negative emotional expression, and problem oversimplification [83]. However, recent studies highlighted that physical neglect was as damaging as abuse since it disrupted early peer- or parent-child relationships and thus reinforced invalidating environments [84]. Emerging studies indicated the role of exposure to parental maltreatment – including neglect – in a general experience of invalidating environment [85].
5. LIMITATIONS
There are several limitations to this study. First, the cross-sectional design limits the ability to establish the causal relationship between psychotic symptoms and childhood trauma among individuals with BPD. Second, the reliance on self-reported measures for psychotic experiences and childhood trauma may introduce recall bias and affect the accuracy of the data. Third, the snowball and convenience sampling method employed in the study may have introduced selection bias, as participants were not randomly selected. This limits the representativeness of the sample, increasing the likelihood that the types of childhood trauma, along with the psychotic experiences and distress, may be overrepresented or underrepresented among our study participants. Additionally, the prevalence of females in the sample and the geographical restriction to Egypt may limit the generalizability of our findings to other populations. Despite these limitations, the study gives insights into the complex relationship between psychotic experiences and childhood trauma in individuals with BPD.
CONCLUSION
The study findings provide evidence for the strong associations between psychotic experiences, their severity (distress), and childhood trauma among individuals with BPD. Individuals with BPD reported significantly higher levels of all types of childhood trauma compared to controls. The differential analysis of the specific influence of childhood trauma types on BPD and its psychotic symptoms identified that sexual abuse and physical neglect strongly predicted the latter. Furthermore, physical neglect emerged as the strongest predictor of both BPD and psychotic symptoms.
By integrating Linehan’s Biosocial Model with trauma theory, this study highlighted that early physical neglect – often overlooked in BPD models – may strongly contribute to shaping invalidating environments and thus influencing BPD symptom expression. Therefore, this study provides culturally relevant insights into the differential role of childhood trauma in BPD development and psychotic distress in non-western contexts. These findings emphasize the importance of trauma-informed interventions, particularly addressing early neglect-related adversity, to reduce the risk of severe psychotic symptoms in BPD individuals.
UNRESOLVED QUESTIONS AND FUTURE RESEARCH DIRECTIONS
Nevertheless, several unresolved questions remain, which may be the focus of further research. For instance, the specific mechanisms through which neglect contributes to psychotic symptoms – through neurobiological dysregulation, invalidation, and/or maladaptive coping strategies – need deeper examination. Additionally, examining cultural differences in the differential impact of trauma types on BPD and its symptom expression would contribute to the generalizability of findings.
THEORETICAL IMPLICATIONS
This study expands existing literature by integrating physical neglect within the invalidating environment framework of Linehan’s Biosocial Theory of BPD development [56]. This suggests that lack of basic caregiving, physical support, and neglect-related childhood trauma may disrupt emotion regulation, enabling maladaptive coping mechanisms. Although recent studies have begun to examine the role of physical neglect within invalidating environments, they are not directly related to BPD and psychotic experiences. By filling this gap, the present study contributes to the yet limited discourse on how neglect-specific trauma contributes to shaping an invalidating environment and thus uniquely impacts BPD symptom expression.
Furthermore, this study contributes to understanding BPD development and its psychotic symptoms within the trauma theory framework by highlighting the differential effects of childhood trauma types. While most studies have focused on the effects of sexual and physical abuse on BPD, this study shows that physical neglect is a distinct predictor of BPD and psychosis. Additionally, by examining this association in an Egyptian sample, the study broadens the literature on trauma and psychotic distress in non-Western populations, where cultural differences in caregiving and child trauma exposure may influence BPD symptom expression.
PRACTICAL IMPLICATIONS
These findings offer several practical interdisciplinary applications in the areas of mental health, social work, and education. Given that physical neglect emerges as a key predictor of BPD and psychotic symptoms, neglect-specific psychological assessments could be employed in addition to the traditional diagnostic frameworks to enhance early identification. Besides, trauma-informed interventions addressing BPD symptomology may specifically focus on neglect-related vulnerabilities through attachment-based therapies and resilience-building techniques, to mitigate long-term psychological effects of childhood adversity.
Since individuals with BPD who experience early physical neglect and other childhood trauma often develop social withdrawal and distorted perceptions of interpersonal relationships, these maladaptive patterns may reinforce emotional dysregulation and unstable relational dynamics. Community-based support and relational interventions may counter these effects by promoting social resilience and adaptive coping strategies. This may mitigate long-term psychological consequences associated with BPD.
Finally, in the field of educational psychology, these findings emphasize the critical role of early intervention within school settings, highlighting the need for incorporating early intervention programs in child-protection policies at schools and caregiver education to reduce long-term mental health consequences of early deprivation. In particular, social-emotional learning (SEL) programs may offer structured emotional regulation support for students from adverse childhood backgrounds. Moreover, training teachers and school counsellors to recognize trauma-related behavioral patterns and implement supportive, inclusive classroom strategies may serve as a protective mechanism against further psychosocial deterioration in individuals at risk of BPD development.
AUTHOR’S CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: J.K.: Data Analysis or Interpretation; M.A.Z., J.K., R.A.N.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| BPD | = Borderline Personality Disorder |
| BSL-23 | = The Borderline Symptom List |
| PQ-B | = The 21-item Prodromal Questionnaire, Brief Version |
| CTQ | = The 28 item Childhood Trauma Questionnaire–Short Form |
| GLM | = Generalized Linear Model |
| AMOS | = Analysis of Moment Structures |
| HPA | = Hypothalamic Pituitary Adrenal |
| SEL | = Social Emotional Learning |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval for the study was granted by the Faculty of Arts and Humanities (FOAH) Ethics Committee at the British University in Egypt under the approval No. 24-1112.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All participants provided informed consent prior to data collection, in line with institutional and established ethical standards. As no personal or identifiable information was collected or published, specific consent for publication was not required. Data were anonymized and presented in aggregate, ensuring participant confidentiality.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Open Science Framework (OSF) at https://osf.io/ctga9/, reference number DOI 10.17605/OSF.IO/CTGA9.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the effort and contributions of our research assistant, Martina Helmy, in collecting important data to support this research.