RESEARCH ARTICLE
Impact of COVID-19 Pandemic on the Psychological Status of Palestinian Adults in the West Bank, Palestine; A Cross-Sectional Study
Imad T. Asmar1, Hani Naseef 2, *, Nimeh Al-Shami2, Maram K. Jaghama1, Abdallah D. Abukhalil2, Areefa A. Karsh1, Fuad A. AlFayyah1, Ro'a M. Dagher1
Article Information
Identifiers and Pagination:
Year: 2021Volume: 14
First Page: 227
Last Page: 237
Publisher ID: TOPSYJ-14-227
DOI: 10.2174/1874350102114010227
Article History:
Received Date: 2/12/2020Revision Received Date: 28/4/2021
Acceptance Date: 28/5/2021
Electronic publication date: 05/10/2021
Collection year: 2021

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Coronavirus Disease 2019 (COVID-19) rapid manifestation and spread have disrupted world norms and affected people's daily activities and life. Many ministries chose mass lockdown protocol as a way to control the virus spread. Though this protocol has shown to be effective in limiting the Virus transmission, it might have a negative impact on the population's psychological status, such as boredom, confusion, psychological stress, anxiety, depression, and physical effects.
Objective:
This study aimed to find the impact of the COVID-19 pandemic on the Palestinian adults' psychological status by assessing the participant's practices, reports of anxiety and depression during the pandemics
Methods:
An observational descriptive cross-sectional study was conducted among Palestinian adults in the West Bank, at the occupied Palestinian territories, between July and September 2020. The questionnaire was structured into two domains: the first domain includes nine questions about sociodemographic data. The second consisted of 33 (yes and no) questions evaluating the participant's psychological status.
Results:
739 participants with a mean age of 31.76, filled the online questionnaire. Around one-third of respondents revealed having many signs of anxiety, and around 42% of respondents expressed having many signs of depression. Females were significantly more likely to have signs of depression, whereas front-line COVID-19 health care workers were significantly the least likely to have signs of depression and no signs of depression were found among participants with high incomes.
Conclusion:
COVID-19 pandemic has a negative effect on mental status; most participants have signs of anxiety and depression.
1. INTRODUCTION
One of the most significant medical challenges nowadays is the Coronavirus Disease 2019 (COVID-19) outbreak caused by a strain of SARS– CoV 2 [1]. This pandemic started in late December 2019 in Wuhan city, China [2], and became an international problem and public health concern for many countries. Many ministries chose mass lockdown protocol to control the virus spread [3]. The lockdown method negatively affected the global economy, with a decline reported in different economic sectors, reflecting on the individuals' lives [4]. Moreover, the rapid continuous spread of Coronavirus along with the protective measures to prevent virus transmissions, such as maintaining social distance, strict isolation, and quarantine, are associated with a negative impact on the public's psychological status and mental health [5] due to the increase in the general sense of boredom and their confusion about time [6]. Moreover, fear of the COVID-19 pandemic, the forced lockdown, and economic deterioration brought great psychological stress, anxiety, and depression among the population, adding to its morbidity and mortality [4, 7, 8].
The literature shows a great deal of emphasis on identifying the virus's pathogenicity, transmission mode, clinical symptoms, clinical outcomes, treatments, and vaccine development, while the psychological effect was neglected [4, 9]. Psychological effects and signs of mental illness are characteristic of rapidly spread infection diseases [10]. Furthermore, the pandemic psychological effects are more pronounced and long- lasting compared to physical signs and symptoms [11]. After COVID- 19 deceleration in China, both negative emotions and social risk sensitivity increased, while positive emotions decreased [12]. Many studies were conducted to investigate the COVID- 19 pandemics' psychological effect and concluded that many mental health problems manifested among different communities, including stress, anxiety, fear, and anger [9]. Health care providers and females have the highest risk for psychological issues and mental health problems [13,14]. In an Italian study, higher scores of worries for different causes were reported among the Italian population; the anxiety and stress levels were above normal ones [15].
Moreover, participants in a study among the Indian population reported higher anxiety, sleep disturbance, distress, and paranoia about acquiring COVID-19 infection [16]. In a cross-sectional study in West Bengal, the respondents felt more worried, depressed, sleep disturbed, and took hydroxy- chloroquine as prophylaxis from COVID-19 [17]. Fear of death and feeling lonely were the main psychological effects that concerned COVID-19 infected patients [18].
Recently, several studies have been conducted to evaluate the pandemic’s psychological effect and the impact of the COVID-19 outbreak on different segments of the population since the initial outbreak [ 2,19–22]. A cross-sectional study conducted in Saudi Arabia [23] included 878 participant and showed that the majority of participants (67.6%) had a moderate level of stress related to COVID-19 lockdown, which has a significant effect on participant’s mental and physical quality of life. Firdous et al. (2021) [24] demonstrated that anxiety among females was significantly higher than males. The prevalence of depression was also higher among females, with no significant difference among genders during the COVID-19 pandemic. The study concluded that the mental well-being of health workers within the frontlines is crucial for sustainable health care services in medical care, and the psychological problems during the COVID-19 outbreak global disaster need special attention. One Italian study [25], in particular, examines the effect of government lockdown and restriction on mental health and stress. Mild/severe levels of depression almost doubled after lockdown from 15.39% before lockdown to 32.30% after lockdown. The study concluded that cognitive and mental health changes due to COVID-19 lockdown lead to higher severity and prevalence of depression, anxiety disorders, and other psychological issues involving lesser sleep, appetite, libido, and hypochondria. In a survey of the Chinese population conducted in the first two weeks after the COVID-19 outbreak, 53.8% said the outbreak had a mild to extreme psychological effect, with 28.8% reporting moderate to severe anxiety symptoms and 8.1% reporting moderate to severe stress levels [2]. According to a survey of the Indian people, the prevalence of anxiety was 3.29%, obsession 13.47%, and fear 46.9% [26].
In the Arabic region, limited number of studies have been conducted, including; Saudi Arabia, Kuwait and Bahrain, to assess the pandemic psychological effect and the impact of the COVID-19 outbreak on the general population [27-30] and another two studies have been conducted in Oman and Egypt on subgroups such as healthcare workers [31, 32]. These studies' findings revealed the presence of stress, anxiety, and depression symptoms at variable degrees
In Palestine, the first case of COVID-19 was diagnosed in the city of Bethlehem in March 2020. Palestinian health ministries have taken steps to limit the virus's spread by closing towns, counties and restrict people's movement. These steps were very successful in keeping the pandemic curve down; on the other hand, living with the fear of COVID-19 infection and closure protocols significantly impacted people's lives and psychological well-being. Locally, there have been no studies in Palestine that assess the psychological impact of the COVID-19 outbreak and its protective measures imposed. This study aims to find the impact of the COVID-19 pandemic on the Palestinian adults' psychological status by assessing the participant's practices, reports of anxiety, and depression during the pandemics.
2. MATERIALS AND METHODS
2.1. Study Design and Sample
An observational descriptive cross- sectional study was conducted among Palestinian adults in the West Bank, at the occupied Palestinian territories, between July and September 2020. The data were collected through an online distributed questionnaire. The questionnaire was designed and provided by Google Forms (Google Inc., USA) under the supervision of an Informational Technology Department personnel. The total population presented was around two million adults [33]. The sample size was 385 as calculated online with a 95% confidence level and a 5% error margin [34]. 739 respondents filled the questionnaire. All adults, West Bank dwellers and having internet access were allowed to participate in the study. Participants currently suffering or previously infected with COVID-19 were excluded from the study due to the stress and anixiety caused from the disease itself. Furthermore, participants who did not believe in the virus's presence were excluded. The IRB committee at the Faculty of Pharmacy, Nursing and Health Professions, Birzeit University, approved this study, with reference number BZU-PNH-2009.
2.2. Study Tool
The questionnaire was developed after reviewing similar international studies [17, 27]. The questionnaire’s components were reviewed and evaluated by the researchers’ team. The questionnaire’s content relevance, validity, and appropriateness were verified by four multidisciplinary expert panels with experience in epidemiology and research from the Faculty of Pharmacy, Nursing, and Health Professions at Birzeit University. Based on experts' feedback, some questionnaire items were excluded, and specific questions were re-phrased. The questionnaire was written in the English language, then translated into the Arabic language by experts. It was revised by an epidemiologist from the Faculty of Pharmacy, Nursing, and Health Professions. Five experts and professionals reviewed the questionnaire components for content validity, relevance, and appropriateness. Then, a pilot study was conducted among 42 participants to check the questionnaire clarity. Accordingly, the questionnaire's final version was structured into two domains: the first domain includes nine questions about sociodemographic data. The second consisted of 33 (yes and no) questions evaluating the participant's psychological status, information source, and the time spent during COVID-19 exposure; furthermore, an additional option of “I don't know” was added in some questions.
2.3. Statistical Analysis
All questions were coded, imported to IBM SPSS Statistics 22 for analysis, and recoding for questions with more than two choices was performed to answer a Yes/ No basis. Principle Component Analysis (PCA) with varimax rotation was performed to extract factors using the loading criteria of 0.40. Twenty-six items were examined, divided into three subscales; 9 items as anxiety signs, seven items as depression signs, nine items reflect participants' practices, and an item related to anxiety due to income loss was deleted. Then, the reliability coefficient (Cronbach α) for each subscale was calculated and showed good internal consistency for depression (α=0.803), anxiety (α=0.762), and acceptable for practice (α=0.555). It is important to note that the presence of those anxiety or depression signs does not reflect a clinical diagnosis of anxiety or depression.
| Sociodemographic Characteristics | N (%) | |
|---|---|---|
| Gender | Male | 297 (42.8) |
| Female | 397 (57.2) | |
| Age (years) | Less than 21 | 175 (25.2) |
| 21-30 | 230 (33.1) | |
| 31-40 | 122 (17.6) | |
| More than 40 | 167 (24.1) | |
| Marital status | Single | 365 (52.6) |
| Married | 312 (45.0) | |
| Others | 17 (2.4) | |
| Governorate | Jerusalem and the occupied Palestinian territory | 116 (16.7) |
| North of the WB | 191 (27.5) | |
| Middle of the WB | 310 (44.7) | |
| South of the WB | 77 (11.1) | |
| Place of residency | City | 363 (52.3) |
| Village | 313 (45.1) | |
| Refugee camp | 18 (2.6) | |
| Educational attainment | Uneducated or Less than Secondary post-compulsory education | 31 (4.5) |
| Secondary post- compulsory education |
79 (11.4) | |
| Diploma | 47 (6.8) | |
| Bachelor's degree | 411 (59.2) | |
| Higher education | 126 (18.2) | |
| Occupation | Health sector | 107 (15.4) |
| Non- Health sector | 252 (36.3) | |
| Student | 254 (36.6) | |
| Unemployed | 81 (11.7) | |
| Occupation type | Employee | 258 (37.2) |
| personal business | 112 (16.1) | |
| Not applicable | 324 (46.7) | |
| Financial income | Increased | 9 (1.3) |
| Steady | 144 (20.7) | |
| Decreased | 403 (58.1) | |
| Not applicable | 138 (19.9) | |
Descriptive statistics were performed to present data. For anxiety and depression subscales, count for yes answers, which reflect that sign's presence, was performed and scored 1 for each. Recoding for the total anxiety scale score was subdivided into almost having no anxiety signs (0-2), having some anxiety signs (3-6), and having many anxiety signs (7-9). For the depression scale, the total score was subdivided into almost having no depression signs (0-2), having some depression signs (3-5), and having many depression signs (6-7). Chi-square testing with a 95% confidence interval was run to identify any association between the sociodemographic data and the other three questions related to direct deal with COVID-19 patients with the anxiety and depression subscales.
3. RESULTS
3.1. Sociodemographic Characteristics of Study Participants (N = 694)
A total of 739 participants completed the on-line questionnaire. 39 (5.3%) participants did not believe in the existence of virus COVID-19, and 6 (0.8%) were infected with COVID-19. Of those 694 remaining participants aged between 18 to 80 with a mean age 31.76, 57.2% were females, and 52.6% were single. Almost 44.7% of the participants resided in the middle of the West Bank with 52.3% city residents. More than half of the participants 59.2% were holders of Bachelor, 58.1% had decreased monthly income due to the pandemic, and only 15.4% were healthcare workers (Table 1). Additionally, 90.9% of respondents reported that they did not deal with an infected patient with COVID-19, 94.7% of respondents reported that they did not assist in providing health care to a person who was diagnosed with COVID-19, and 47.7% revealed that there are no confirmed cases of COVID- 19 in their neighborhood. These three variables are identified as independent variables.
Regarding participants' information resources (Fig. 1), the majority (64.4%) relied on the official media outlets in Palestine (Ministry of Health website and government spokesperson), followed by those (62%) who relied on social media, and 50.6% on scientific resources such as the World Health Organization, International Centers for Disease Control and Prevention or scientific papers.
Furthermore, when we asked them about their time, how they have spent during the complete closure of the West Bank (Fig. 2), more than half were busy doing household chores, engaged in social media, or only lying and sleeping, while only 36.3% revealed that they were working from home.
3.2. Anxiety
Around one- third of respondents (35.2%) have many signs that reflected their feeling of anxiety (Fig. 3). Most participants (83.1%) felt anxious due to the lack of an effective treatment or vaccination for COVID-19, (75.9%) were anxious regarding the limited capabilities and tools of the local authorities to combat the COVID-19 pandemic, and (64.3%) of participants have felt anxious more than usual since the beginning of the pandemic. On the other hand, more than half of the participants had no changes in their sleep cycle, did not become obsessed about getting infected with COVID-19, and did not become more irritable and angry than usual with percentages of 65.7%, 59.4%, and 55.9% respectively. Worries and anxieties about the financial losses and future of family members during the quarantine were concerns of participants with a percentage of 84.4% and 83.6% respectively (Table 2).
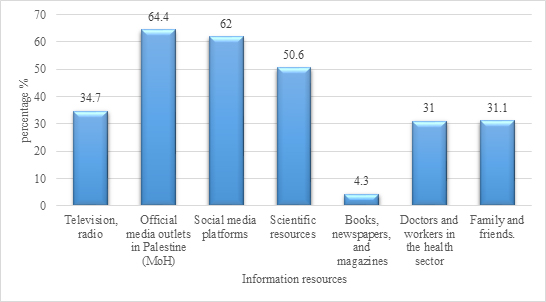 |
Fig. (1). The participants' resources of information about COVID-19. (N=694). |
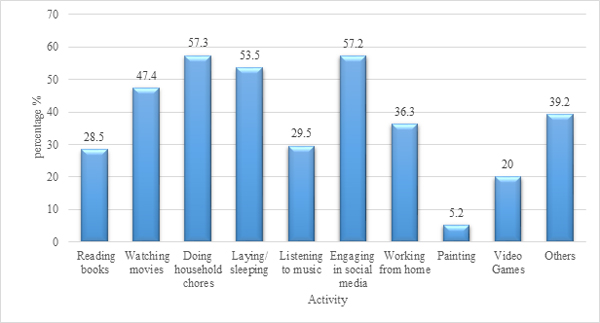 |
Fig. (2). The activities participants spent their time in. (N=694). |
| Statement | Yes n (%) | No n (%) |
|---|---|---|
| Have you felt anxious more than usual since the beginning of the pandemic in Palestine? | 446 (64.3) | 248 (35.7) |
| Do you always think about getting infected with COVID-19 since the beginning of the epidemic in Palestine? | 282 (40.6) | 412 (59.4) |
| Has there been a change in your sleep cycle since the beginning of the pandemic in Palestine? | 238 (34.3) | 456 (65.7) |
| Have you felt anxious about the limited capabilities and tools of the local authorities to combat the COVID 19-pandemic? | 527 (75.9) | 167 (24.1) |
| Have you felt anxious due to the lack of an effective treatment or vaccination for COVID-19? | 577 (83.1) | 117 (16.9) |
| Have you been concerned about your future and that of your family members since the beginning of the pandemic in Palestine? | 586 (84.4) | 108 (15.6) |
| Have you become more irritable and angry than usual since the beginning of the pandemic in Palestine? | 306 (44.1) | 388 (55.9) |
| Did you become more anxious when you got information about COVID-19? (From WhatsApp, Facebook, Television, Radio ..... etc.) | 498 (71.8) | 196 (28.2) |
| Have you ever felt anxious about the society's perception if you are infected with the Coronavirus? | 253 (36.5) | 441 (63.5) |
| Have you felt anxious about the financial loss you suffered during the lockdown/quarantine in the West Bank? | 580 (83.6) | 114 (16.4) |
Table 3 shows Chi- square results, which revealed a significant difference between the anxiety signs at different ages (P- value= 0.024). Younger respondents aged less than 21 years were less likely to have many anxiety signs (26.9%) compared with older aged 21 to 30 (37.0%), 31 to 40 (34.4%), and over 40 (41.9%). Also, respondents who stated that there were not any confirmed cases of COVID-19 in the neighborhood were significantly less likely to have many anxiety signs (26.6%, P-value< 0.001) compared to those who had cases or do not know about their neighbors (44.6% and 40.2%), respectively. No significant associations were found between having anxiety signs and the respondent's sex, educational attainment, place of residency, occupation, providing care for COVID-19 infected patients, and their income during the spread of the virus.
3.3. Depression
Regarding depression signs, (41.6%) of respondents expressed having many depression signs (Fig. 3), a high percentage of the participants reported that COVID- 19 had affected their mental status negatively and they felt depressed since the beginning of the pandemic in Palestine with percentages of 71.2% and 60.8% respectively. Furthermore, half of the participants (50.1%) felt depressed due to the changes in some social behaviors and habits, and 63.3% became more depressed when they got information about COVID-19. Adapting and adjusting daily life to the lockdown protocol caused depression for 70.5% of the participants, 66.7% felt depressed due to their commitment at home during the lockdown, and 59.2% of the respondents believed that the COVID-19 pandemic would pose a threat to their existence.
Table 3. Distribution of different respondents' characteristics with the anxiety signs they had.
| Sociodemographic Characteristics | Anxiety Signs | P-value | |||
|---|---|---|---|---|---|
| Having Almost No Signs | Having Some Signs | Having Many Signs | |||
| Gender | Male | 47 (15.8) | 145 (48.8) | 105 (35.4) | 0.226 |
| Female | 46 (11.6) | 212 (53.4) | 139 (35.0) | ||
| Age (years) | Less than 21 | 32 (18.3) | 96 (54.9) | 47 (26.9) | 0.024 |
| 21-30 | 26 (11.3) | 119 (51.7) | 85 (37.0) | ||
| 31-40 | 11 (9.0) | 69 (56.6) | 42 (34.4) | ||
| More than 40 | 24 (14.4) | 73 (43.7) | 70 (41.9) | ||
| Marital status | Single | 55 (15.1) | 194 (53.2) | 116 (31.8) | 0.301 |
| Married | 37 (11.9) | 154 (49.4) | 121 (38.8) | ||
| Others | 1 (5.9) | 9 (52.9) | 7 (41.2) | ||
| Governorate | Jerusalem and the oPt | 14 (12.1) | 67 (57.8) | 35 (30.2) | 0.393 |
| North of the WB | 27 (14.1) | 99 (51.8) | 65 (34.0) | ||
| Middle of the WB | 41 (13.2) | 160 (51.6) | 109 (35.2) | ||
| South of the WB | 11 (14.3) | 31 (40.3) | 35 (30.2) | ||
| Place of residency | City | 57 (15.7) | 187 (51.5) | 119 (32.8) | 0.374 |
| Village | 34 (10.9) | 161 (51.4) | 118 (37.7) | ||
| Refugee camp | 2 (11.1) | 9 (50.0) | 7 (38.9) | ||
| Educational attainment | Uneducated or Less than Secondary post-compulsory education | 4 (12.9) | 12 (38.7) | 15 (48.4) | 0.216 |
| Secondary post- compulsory education |
17 (21.5) | 32 (40.5) | 30 (38.0) | ||
| Diploma | 7 (14.9) | 22 (46.8) | 18 (38.3) | ||
| Bachelor’s degree | 51 (12.4) | 222 (54.0) | 138 (33.6) | ||
| Higher education | 14 (11.1) | 69 (54.8) | 43 (34.1) | ||
| Occupation | Health sector | 15 (14.0) | 52 (48.6) | 40 (37.4) | 0.107 |
| Non- Health sector | 28 (11.1) | 120 (47.6) | 104 (41.3) | ||
| Student | 41 (16.1) | 140 (55.1) | 73 (28.7) | ||
| Unemployed | 9 (11.1) | 45 (55.6) | 27 (33.3) | ||
| Occupation type | Employee | 29 (11.2) | 137 (53.1) | 92 (35.7) | 0.556 |
| personal business | 16 (14.3) | 52 (46.4) | 44 (39.3) | ||
| Not applicable | 48 (14.8) | 168 (51.9) | 108 (33.3) | ||
| Financial income | Increased | 2 (22.2) | 4 (44.4) | 3 (33.3) | 0.079 |
| Steady | 24 (16.7) | 82 (56.9) | 38 (26.4) | ||
| Decreased | 46 (11.4) | 198 (49.1) | 159 (39.5) | ||
| Not applicable | 21 (15.2) | 73 (52.9) | 44 (31.9) | ||
| Deal directly with an infected COVID-19 patient | Yes | 9 (14.3) | 36 (57.1) | 18 (28.6) | 0.513 |
| No | 84 (13.3) | 321 (50.9) | 226 (35.8) | ||
| Assist to provide health care to a diagnosed COVID-19 patient | Yes | 7 (18.9) | 19 (51.4) | 11 (29.7) | 0.544 |
| No | 86 (13.1) | 338 (51.4) | 233 (35.5) | ||
| Presence of confirmed cases in the neighborhood | Yes | 18 (7.8) | 110 (47.6) | 103 (44.6) | <0.001 |
| No | 53 (16.0) | 190 (57.4) | 88 (26.6) | ||
| Do not Know | 22 (16.7) | 57 (43.2) | 53 (40.2) | ||
As shown in Table 4, a significant association between the signs of depression the respondents had and their sex (P-value= 0.001), the females (46.3%) were more likely to have many depression signs compared to males (35.4%). Interestingly, workers at health sectors (29.9%, P-value= 0.039), those who deal directly with confirmed cases of COVID-19 (19.0%, P-value= 0.001), and those who assist in providing health care for a diagnosed COVID-19 (16.2%, P-value= 0.003) patient were significantly less likely to have many depression signs compared to others. Regarding the participants' income, those with increased income were significantly more likely to have almost no signs of depression (55.6%, P-value=0.007) compared to whose income does not change, decrease, or have no income (30.6%, 20.8%, 23.9%) respectively.
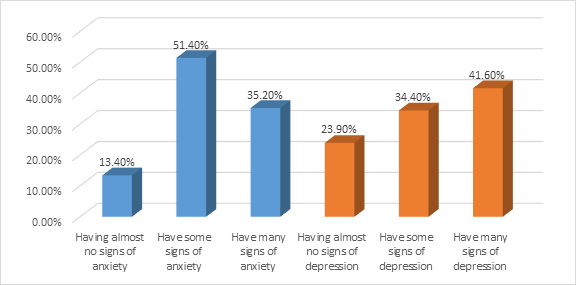 |
Fig. (3). Percentage of participants with signs of anxiety and depression. |
| Sociodemographic Characteristics | Depression Signs | P-value | |||
|---|---|---|---|---|---|
| Having Almost No Signs | Having Some Signs | Having Many Signs | |||
| Gender | Male | 91 (30.6) | 101 (34.0) | 105 (35.4) | 0.001 |
| Female | 75 (18.9) | 138 (34.8) | 184 (46.3) | ||
| Age (years) | Less than 21 | 40 (22.9) | 65 (37.1) | 70 (40.0) | 0.126 |
| 21-30 | 44 (19.1) | 86 (37.4) | 100 (43.5) | ||
| 31-40 | 29 (23.8) | 38 (31.1) | 55 (45.1) | ||
| More than 40 | 53 (31.7) | 50 (29.9) | 64 (38.3) | ||
| Marital status | Single | 76 (20.8) | 130 (35.6) | 159 (43.6) | 0.180 |
| Married | 84 (26.9) | 106 (34.0) | 122 (39.1) | ||
| Others | 6 (35.3) | 3 (17.6) | 8 (47.1) | ||
| Governorate | Jerusalem and the oPt | 29 (25.0) | 40 (34.5) | 47 (40.5) | 0.272 |
| North of the WB | 50 (26.2) | 58 (30.4) | 83 (43.5) | ||
| Middle of the WB | 71 (22.9) | 120 (38.7) | 119 (38.4) | ||
| South of the WB | 16 (20.8) | 21 (27.3) | 40 (51.9) | ||
| Place of residency | City | 97 (26.7) | 125 (34.4) | 141 (38.8) | 0.319 |
| Village | 66 (21.1) | 106 (33.9) | 141 (45.0) | ||
| Refugee camp | 3 (16.7) | 8 (44.4) | 7 (38.9) | ||
| Educational attainment | Uneducated or Less than Secondary post-compulsory education | 6 (19.4) | 11 (35.5) | 14 (45.2) | 0.295 |
| Secondary post- compulsory education |
25 (31.6) | 23 (29.1) | 31 (39.2) | ||
| Diploma | 10 (21.3) | 18 (38.3) | 19 (40.4) | ||
| Bachelor’s degree | 86 (20.9) | 144 (35.0) | 181 (44.0) | ||
| Higher education | 39 (31.0) | 43 (34.1) | 44 (34.9) | ||
| Occupation | Health sector | 35 (32.7) | 40 (37.4) | 32 (29.9) | 0.039 |
| Non- Health sector | 62 (24.6) | 75 (29.8) | 115 (45.6) | ||
| Student | 54 (21.3) | 90 (35.4) | 110 (43.3) | ||
| Unemployed | 15 (18.5) | 34 (42.0) | 32 (39.5) | ||
| Occupation type | Employee | 72 (27.9) | 90 (34.9) | 96 (37.2) | 0.138 |
| personal business | 30 (26.8) | 36 (32.1) | 46 (41.1) | ||
| Not applicable | 64 (19.8) | 113 (34.9) | 147 (45.4) | ||
| Financial income | Increased | 5 (55.6) | 1 (11.1) | 3 (33.3) | 0.007 |
| Steady | 44 (30.6) | 57 (39.6) | 43 (29.9) | ||
| Decreased | 84 (20.8) | 138 (34.2) | 181 (44.9) | ||
| Not applicable | 33 (23.9) | 43 (31.2) | 62 (44.9) | ||
| Deal directly with an infected COVID-19 patient | Yes | 22 (34.9) | 29 (46.0) | 12 (19.0) | 0.001 |
| No | 144 (22.8) | 210 (33.3) | 277 (43.9) | ||
| Assist to provide health care to a diagnosed COVID-19 patient | Yes | 15 (40.5) | 16 (43.2) | 6 (16.2) | 0.003 |
| No | 151 (23.0) | 223 (33.9) | 283 (43.1) | ||
| Presence of confirmed cases in the neighborhood | Yes | 45 (19.5) | 82 (35.5) | 104 (45.0) | 0.104 |
| No | 91 (27.5) | 117 (35.3) | 123 (37.2) | ||
| Do not Know | 30 (22.7) | 40 (30.3) | 62 (47.0) | ||
3.4. Practice
The majority of respondents (92.1%) have not visited a doctor or took a COVID-19 test to confirm their potential infection, and 87.3% have not carried out any laboratory tests to ensure that they are healthy. Simultaneously, around two- thirds of participants (63.3%) checked their fever since the pandemic in Palestine, and the vast majority of participants (97%) have not requested the help of a psychiatry helpline to reduce their anxiety or depression during the pandemic. Most participants have not taken any prophylactic medication (hydroxychloroquine or dexamethasone) or antibiotics for COVID- 19 infection, with a percentage of 99.1% and 96.5%, respectively. Furthermore, the majority of the participants (90.6%) had not taken any sleep medication, and (96.3%) are not on any antidepressant(s)/ anti-anxiety medication since the beginning of the pandemic in Palestine.
4. DISCUSSION
People in the community face several challenges during the pandemics phenomenon. The impacts of these pandemics are often severe, which may negatively affect a given population's mental health. The depression and anxiety related to pandemics also influence the behavior of people in the community. Hence, this study attempted to evaluate the psychological impact of the COVID-19 pandemic on Palestinian adults in the West Bank.
The study results related to anxiety revealed that one- half of the respondents showed some signs of anxiety, whereas one- third have many signs. There was a debate on assessing anxiety in the literature, whether using a specific anxiety scale such as the Hamilton Anxiety Rating scale or any other possible way. However, many studies showed a modest interesting mean, percentages, and significance values for respondents who became anxious due to the COVID-19 pandemic, and almost one-third to one- half of the respondents in these studies became anxious [35, 36]. Younger respondents aged less than 21 years were less likely to have many anxiety signs compared to older respondents, that consistent with recent studies [37]. Younger adults have less financial responsibility, less comorbidity, keep a busy lifestyle to distract their thoughts away from COVID-19, unlike the older respondents who might experience fear of falling sick or dying. Respondents with no confirmed COVID-19 cases in their neighborhood were less likely to have many anxiety signs versus those who have cases in the neighborhood or do not know about their neighbor's infection status, and these results are similar to a study conducted by Sue et al. [38]. Increasing anxiety levels are due to the fear of getting infected with the virus due to the risk of social contact or livening proximity with an infected neighbor.
As far as depression, the study results showed that front line health care workers who interacted directly with confirmed COVID-19 cases are less likely to have many depression signs. These results are contrary to literature findings were health care workers revealed poor mental health because of COVID- 19, which had a negative impact on their well- being and quality of care provided to patients and most front- line healthcare workers reported high levels of stress and depression compared to other workers [39]. However, this finding has limitations and can not be generalized due to the small number of healthcare workers participating in the study.
Regarding gender, females have a more negative psychological impact than males due to the COVID-19 pandemic. This finding is similar to other studies stating that females are more likely to be affected or exposed to negative psychological consequences such as depression [40]. That might be due to several reasons related to the nature of the local community's prevailing culture, such as the dependence on the distance education system, overthinking about the financial situation, and being unemployment. Women have a different hormonal system that in stressful situations such as the COVID-19 pandemics emotionally responded in different way.
Moreover, financial stability and increased income have an inverse relationship with depression during the pandemic. Respondents with an increased income had no signs of depression compared to those with decreased or unchanged income. Other studies support this finding that respondents with increased income were less depressed compared to others with income instability, either decreased or unchanged during the pandemic [41]; that may be due to the significant stress and responsibilities added on the breadwinner of the family to meet their needs of food and shelter in the case of income instability.
However, regarding self- treatment or infection prophylaxis practice, most of the respondents had not taken either a prophylactic dose of (Hydroxychloroquine or Dexamethasone) or antibiotics, which is inconsistent with the results of other study conducted by Mehra [42]. That may be related to the higher level of education of the sample, that more than half of the participants hold a bachelor's degree. Education make them more aware to the inappropriate practices. Moreover, no conclusive research confirmed that Dexamethasone or Hydroxychloroquine help in preventing or treating COVID- 19, added to the fact that authorities are standing against self- medication with these types of medicine during the pandemic [43].
Furthermore most respondents had not taken either antidepressant, anti-anxiety, or sleep medication during the pandemic to control or treat anxiety, depression, or sleeping disorders. These results are in line with previous research, where the vast majority of respondents have not taken these medications during the COVID-19 outbreak [17].
CONCLUSION
COVID-19 pandemic has a negative effect on mental health; according to the study, most participants have signs of anxiety and depression, and it was more common in the middle age group, elderly and females. Confirmed COVID-19 cases in the neighborhood, not knowing the neighbors' infection status, and decreased income were factors associated with the increased risk of anxiety and depression.
Upon these results, governments, health institutions, and health care providers should provide psychological support, mental health education, counseling, and maybe intervention to vulnerable groups. Furthermore, we recommended taking a break from watching, reading, or listening to the news, including social media, and getting facts from global and local health authority platforms.
Mental health, psychological, and social support during this pandemic are essential components in compacting this pandemic, and it should be available and provided alongside health care services to improve community health and wellbeing.
LIMITATIONS OF THE STUDY
This study is limited to people who own computers, laptops, or smartphones and have a Facebook or WhatsApp account to participate in the research. In Addition, it represents mainly the educated population, so it should not be generalized to the whole population.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease-19 |
| PCA | = Principle Component Analysis |
| SARS-CoV-2 | = Severe Acute Respiratory Syndrome Coronavirus 2 |
| SPSS | = Statistical Package for the Social Sciences |
| PNH | = Faculty Of Pharmacy and Nursing and Health Professions Building |
| BZU | = Birzeit University |
| IRB | = Institutional Review Board |
AUTHORS’ CONTRIBUTIONS
IA and NS design the study, planning and supervised the work, review editing, HS design the study, planning and supervised the work, analysis of the results, review editing, AK,FA,RD and MJ drafted the manuscript, AA review editing. The authors read and approved the final manuscript prior to submission.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the IRB committee at Faculty of Pharmacy, Nursing and Health Professions, Birzeit University, Palestine with reference number BZU-PNH-2009.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
The questionnaire was designed and provided by online Google Form with informed consent attached with questionnaire itself. Participants who filled the questionnaire were understood to have given consent.
AVAILABILITY OF DATA AND MATERIALS
The data analyzed during the current study and support the findings are available from the corresponding author [H.N] on reasonable request.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to express our appreciation to the Professors at the Faculty of Pharmacy, Nursing and Health Professions, Birzeit University, Palestine, for their support and an honest thank you to all who participated in the survey.
REFERENCES
| [1] | Banerjee D. The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian J Psychiatr 2020; 50102014 |
| [2] | Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020; 17(5)E1729 |
| [3] | Lee SA. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud 2020; 44(7): 393-401. |
| [4] | Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord 2020; 277: 55-64. |
| [5] | Brown E, Gray R, Lo Monaco S, et al. The potential impact of COVID-19 on psychosis: A rapid review of contemporary epidemic and pandemic research. Schizophr Res 2020; 222: 79-87. |
| [6] | Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res 2020; 29(4)e13074 |
| [7] | Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020; 287112934 |
| [8] | Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci 2020; 74(4): 281-2. |
| [9] | Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry 2020; 66(4): 317-20. |
| [10] | Medical Association A. Addressing the COVID-19 pandemic in populations with serious mental illness 2020. |
| [11] | Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease 2019. |
| [12] | Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: A study on active weibo users. Int J Environ Res Public Health 2020; 17(6): 2032. |
| [13] | Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020; 7(3)e14 |
| [14] | Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr 2020; 52102066 |
| [15] | Germani A, Buratta L, Delvecchio E, Mazzeschi C. Emerging adults and COVID-19: The role of individualism-collectivism on perceived risks and psychological maladjustment. Int J Environ Res Public Health 2020; 17(10)E3497 |
| [16] | Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr 2020; 51102083 |
| [17] | Chakraborty K, Chatterjee M. Psychological impact of COVID-19 pandemic on general population in West Bengal: A cross-sectional study. Indian J Psychiatry 2020; 62(3): 266-72. |
| [18] | Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatr 2020; 51101990 |
| [19] | González-Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 2020; 87: 172-6. |
| [20] | Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in italy. Int J Environ Res Public Health 2020; 17(13): 4779. |
| [21] | Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int J Environ Res Public Health 2020; 17(9): 3165. |
| [22] | Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res 2020; 289113098 |
| [23] | Hawash MM, Alhazmi AH, Wafik W, Muzammil K, Mushfiq S, Ahmed HA. The association of COVID-19 pandemic stress with health-related quality of life in the kingdom of Saudi Arabia: A cross-sectional analytical study. Front Public Health 2021; 9600330 |
| [24] | Mental health status among Health Care Workers in Primary care exposed to COVID-19 pandemic in North Batinah, Oman Available online: https://www.ejmcm.com/article_9827.html (accessed on Apr 27, 2021). |
| [25] | Fiorenzato E, Zabberoni S, Costa A, Cona G. Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PLoS One 2021; 16(1)e0246204 |
| [26] | Srivastava A, Bala R, Srivastava AK, Mishra A, Shamim R, Sinha P. Anxiety, obsession and fear from coronavirus in Indian population: a web-based study using COVID-19 specific scales. Int J Community Med Public Health 2020; 7: 4570. |
| [27] | Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry 2020; 102152192 |
| [28] | Burhamah W, AlKhayyat A, Oroszlányová M, et al. The psychological burden of the COVID-19 pandemic and associated lockdown measures: Experience from 4000 participants. J Affect Disord 2020; 277: 977-85. |
| [29] | Alsalman A, Mubarak H, Aljabal M, et al. The psychological impact of COVID-19 pandemic on the population of bahrain. SSRN Electronic Journal 2020. |
| [30] | Arafa A, Mohamed A, Saleh L, Senosy S. Psychological impacts of the COVID-19 pandemic on the public in egypt. Community Ment Health J 2020; 1-6. |
| [31] | Badahdah A, Khamis F, Al Mahyijari N, et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psychiatry 2020; 002076402093959 |
| [32] | Corbett GA, Milne SJ, Mohan S, et al. Anxiety and depression scores in maternity healthcare workers during the Covid-19 pandemic. Int J Gynecology & Obsterics 2020; ijgo.13279. |
| [33] | Palestine population. (Demographics, Maps, Graphs) 2020. |
| [34] | Sample size calculator - confidence level, confidence interval, sample size, population size, relevant population - Creative Research Systems 2020. |
| [35] | Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 2020; 33(2)e100213 |
| [36] | Madani A, Boutebal SE, Bryant CR. The psychological impact of confinement linked to the coronavirus epidemic COVID-19 in algeria. Int J Environ Res Public Health 2020; 17(10): 3604. |
| [37] | Gómez-Salgado J, Andrés-Villas M, Domínguez-Salas S, Díaz-Milanés D, Ruiz-Frutos C. Related health factors of psychological distress during the COVID-19 pandemic in spain. Int J Environ Res Public Health 2020; 17(11): 3947. |
| [38] | Su J, Chen X, Yang N, Sun M, Zhou L. Proximity to people with COVID-19 and anxiety among community residents during the epidemic in Guangzhou, China. BJ Psych Open 2020; 6(4)e75 |
| [39] | Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun 2020; 88: 901-7. |
| [40] | Losada-Baltar A, Márquez-González M, Jiménez-Gonzalo L, Pedroso-Chaparro MDS, Gallego-Alberto L, Fernandes-Pires J. [Differences in anxiety, sadness, loneliness and comorbid anxiety and sadness as a function of age and self-perceptions of aging during the lock-out period due to COVID-19]. Rev Esp Geriatr Gerontol 2020; 55(5): 272-8. |
| [41] | Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr 2020; 14(5): 779-88. |
| [42] | Mehra MR, Ruschitzka F, Patel AN. Retraction—“Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis” (The Lancet, (S0140673620311806), (10.1016/S0140-6736(20)31180-6)). The Lancet 2020; 394: 1820. |
| [43] | Siemieniuk RA, Bartoszko JJ, Ge L, et al. Drug treatments for COVID-19: living systematic review and network meta-analysis. BMJ 2020; 370: m2980. |