All published articles of this journal are available on ScienceDirect.
Impact of Dialectical Behavior Therapy on Depression and Anxiety in Patients Following COVID-19 Discharge
Abstract
Introduction:
COVID-19 pandemic has a significant impact on mental health including anxiety and depression and can weaken the immune system and make a person more vulnerable to the disease. Psychotherapy techniques have been effective in reducing these disorders. Therefore, this study aimed to investigate the effect of dialectical behavior therapy on depression and anxiety in patients discharged from COVID-19.
Methods:
It was a randomized controlled trial (RCT). The statistical population consisted of 30 men who underwent COVID -19 disease quarantine. Convenience sampling was used and the patients were randomly assigned to experimental and control groups. In the experimental group, dialectical behavior therapy was performed in 10 sessions of 90 minutes. The Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) were used. Data were analyzed using SPSS 21 software and multivariate analysis of variance.
Results:
There was a significant difference between the mean scores of depression and anxiety in the experimental and control groups (p<0.001). The effect of this treatment on reducing the score of depression was 68% and on reducing the score of anxiety was 54%.
Conclusion:
Dialectical behavior therapy can reduce anxiety and depression in patients with COVID-19 disease. It is suggested that this intervention can be used in psychological treatment programs.
1. INTRODUCTION
The covid-19 disease is the result of a new type of coronavirus that was first reported on December 31, 2019, with the original name of the new coronavirus (nCoV-2019) in Wuhan, China, and later became a pandemic with far-reaching economic, social and health consequences [1]. The severity of the disease now appears to be more than initially estimated [2] and this pandemic could have far-reaching consequences for individuals [3]. While the world is in a state of crisis, a state of fear and anxiety pervades it too, and seems to have brought the world to a standstill [4]. On the other hand, collective tragedies, especially those involving infectious diseases, often exacerbate areas of fear and anxiety that appear to cause widespread disruption in the behavior and welfare of many people in the population [5]. One of the psychological problems during the outbreak of disease is job burnout which causes a lack of energy and vitality [6]. At the time of the outbreak of COVID-19 in a Cross-sectional Study in the Southeast of Iran, in the components of emotional exhaustion, Job Burnout (due to hard work and anxiety caused by COVID-19 among hospital staff), and personal inadequacy, 2.2%, 4.7%, and 5.5% of the society had burnout symptoms, respectively, which increased the level of anxiety and stress [7]. These symptoms can also affect people's mental health, even leading to mental disorders such as PTSD [8].
A cross-sectional study was conducted to assess the mental health of family members of staff in five hospitals in China during the outbreak of Covid-19 disease on February 10-20, 2020. In this study, which involved 822 people, the prevalence of anxiety index among these people was equal to 33.7% and depressive symptoms were equal to 29.3% [9]. In the early stages of coronavirus outbreaks in China, more than half of the respondents reported moderate to severe psychological effects and about one-third moderate to severe anxiety. [10]. Previous findings have shown clear links between epidemic patients with anxiety and increased stress symptoms, infection concerns, health, anxiety, posttraumatic stress, and suicide [11]. In a study of health care workers, Lai et al. reported that the majority of participants in the study showed symptoms of depression, anxiety, insomnia, and distress and that a large number of people experienced clinically significant fear and anxiety during an outbreak [12]. Rumination is a way to respond to anxiety, especially associated with the onset, severity, and persistence of depression [13]. Constantine et al. reported that people with anxiety and depression disorders experience more worry [14].
Another problem in respiratory patients is anxiety, which is a common symptom in patients with chronic respiratory disorders [15]. Clinical anxiety can reduce the quality of life of about 60% of chronic respiratory patients [16]. The Covid-19 epidemic has caused a wave of stress and anxiety around the world. Fear of getting sick is usually seen in chronic and dangerous diseases [17]. Anxiety and fear of the unknown always weaken the human immune perception and increase the level of anxiety of the individual, so little information about Covid-19 disease and its treatment has intensified anxiety about the consequences of this disease [18]. Stress and anxiety can also weaken the human immune system and make a person vulnerable to disease [19].
According to studies, Covid-19 patients have a low psychological tolerance capacity and due to the current state of the disease in the world, these people are highly exposed to psychological disorders such as anxiety and depression [20]. In this regard, reviewing the results of several studies conducted on patients with Covid-19 in China during the spread of the disease, a number of these psychological disorders, including anxiety, depression, emotional changes, and insomnia have been reported in these patients [21, 22].
Psychological disorders generally are prevalent among these patients [23]. Anxiety and depression may also discourage people from acting reasonably in response to illness (immunization, wearing masks, social distancing, etc.). Previous studies showed that psychotherapy techniques are important in diagnosing and reducing the symptoms of anxiety and depression [24-26]. One of these techniques is dialectical behavior therapy which can assess coping and maladaptive problem-solving in these people.
Dialectical behavior therapy considers self-destructive behaviors such as depression, anxiety, and other emotional regulation problems in the form of maladaptive problem solving, and uses techniques to solve clients' life problems in more adaptive ways. In dialectical behavior therapy, there are four sections on training behavioral skills: fundamental holistic awareness, distress tolerance, emotional regulation, and interpersonal efficiency. The goal of dialectical behavior therapy is to facilitate the learning of new skills and extend them to the whole context of life and improve problems related to anxiety and depression [27]. Learning dialectical behavior therapy skills by developing effective coping skills significantly increases a client's ability to achieve positive outcomes and facilitates the reduction of maladaptive behaviors [28]. One of the dialectical behavioral therapy skills is distress tolerance skills, which improves the tolerance of people to negative psychological conditions such as depression and anxiety [29]. Emotion regulation skills are another skill of dialectical behavior therapy, and emotional dysregulation can precede the onset of mental disorders such as anxiety and depression. The relationship between depression and emotional regulation difficulties has been confirmed in studies [30]. The outbreak of Covid-19 has confusing and, with changes in people's living conditions, has had devastating psychological effects, including anxiety and depression. Epidemic crisis conditions can cause negative psychological and social effects that in some way affect the mental health of people in society. Therefore, this study attempted to evaluate the effectiveness of dialectical therapy based on depression and anxiety in Covid-19 patients after hospital discharge.
2. MATERIALS AND METHODS
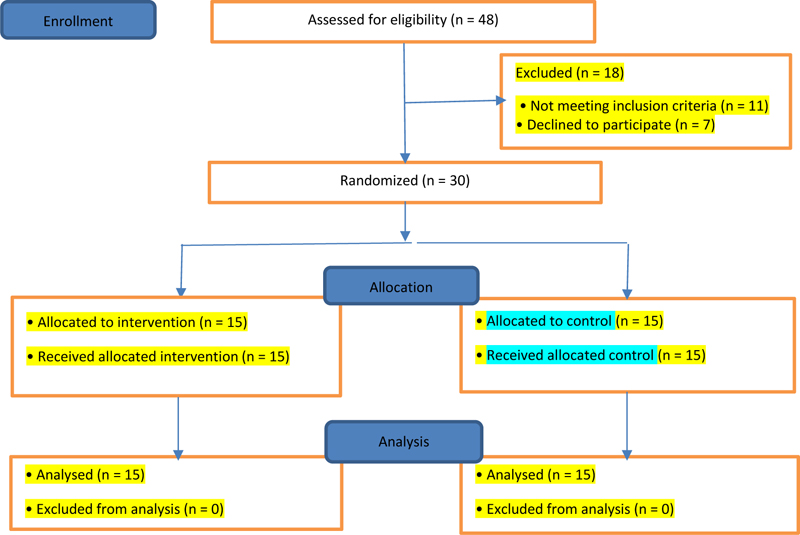
It was a randomized controlled trial (RCT) conducted in Torbate Heydarieh, Iran. This study was approved by the ethics committee of Torbat-e-Heydariyeh University of Medical Sciences and was based on the STROBE guideline. The statistical population included all men who had passed the Covid-19 quarantine period 14 days after their discharge from the hospital. Before starting the intervention, the necessary explanations were given to the individuals about the objectives of the research, and after obtaining the informed consent, the individuals entered the project. The statistical sample consisted of 30 people (15 people in each group) and was determined based on similar studies [31, 32]. The sampling method of this design was Convenience sampling by random assignment in two experimental and control groups. Inclusion criteria were: male gender, minimum age 20 years old, maximum age 40 years [32], no history of chronic mental illness, no use of sedatives, and patients with COVID-19 who have been discharged for 14 days. Exclusion criteria also included: absence of more than two sessions in the training sessions, dissatisfaction and lack of cooperation of individuals, failure to perform the tasks specified in the training process, and recurrence of the disease (based on exclusion criteria, no Person was excluded from the study).
At the beginning of the study, both groups were pretested by Beck Depression Inventory-2 and Beck Anxiety Inventory. The dialectical behavior therapy intervention was performed on the experimental group during 5 weeks in 10 sessions of 9 minutes (two sessions per week) 14 days after their discharge from the hospital in the form of face-to-face sessions with observance of protocols and social distancing and the use of personal protective equipment. The control group was on the waiting list during the treatment intervention. After the last treatment session, a post-test was performed in both groups and the data were analyzed based on a multivariate analysis of variance and SPSS software number 21. One week after the end of the study, dialectical behavior therapy training was held in person for the control group by wearing masks and social distancing. The content of treatment sessions is reported in Table 1.
| Session | Content |
|---|---|
| First | Initial familiarity, statement of purpose of training sessions, duration, number of sessions, and pretest implementation. |
| Second | Overcoming the obstacles of healthy emotions and giving hope skills so that one can understand how emotions affect their thoughts and behaviors. |
| Third | Reducing physical vulnerability to disruptive emotions and how people's thoughts and behaviors can affect their emotions. |
| Fourth | Reducing cognitive vulnerability and perceive how thoughts affect feelings. |
| Fifth | Increasing positive and pleasant emotions (such as happiness) and overcoming negative emotions (such as anger, fear, and sadness) |
| Sixth | Conscious awareness of emotions without judgment (learning to control emotions consciously without judging them, reducing the chances of exacerbation, problems, and emotional distress) |
| Seventh | Coping with emotions (dealing with emotions rather than evading them, which is one of the main goals of the dialectical behavior therapy approach). |
| Eighth | To act against the overwhelming emotion and why we need to understand the feeling. |
| Ninth | Problem Solving (before turbulent feelings become active, emotion regulation) |
| Tenth | Receive feedback from team members on the principles taught, reviewing and summarizing past material and posttest implementation. |
2.1. Beck Depression Questionnaire
This questionnaire consists of 21 items to assess the severity of depression and its diagnosis. Each item has a score between 0 to 3 (never= 0, mild =1, moderate =2 and severe =3) and each person can get a score between 0 to 63. Beck et al. reported internal reliability of 0.73 to 0.92 with a mean of 0.86 and an alpha coefficient of 0.86 for the patient group and 0.81 for the nonpatient group [33]. Dabson and Mohammad Khani obtained 92% reliability of the Persian version of the questionnaire by Cronbach's alpha method. In addition, its structural validity has been confirmed and the retest coefficient has been reported to be 0.49 at three-week intervals [34].
2.2. Beck Anxiety Questionnaire (BAI)
It consists of 21 items, and each statement reflects one of the symptoms of anxiety. This scale is scored as a score between 0 to 3 (never= 0, mild =1, moderate =2 and severe =3). Thus, the range of anxiety scores is from 0 to 63. Concurrent validity of state anxiety, trait anxiety, daily anxiety, and Beck depression questionnaires were 0.58, 0.47, 0.54, and 0.50, respectively, and its internal consistency coefficient was 0.92 and its retest coefficient was 0.81 (,1 week apart) [35]. In the Persian version, the structural validity of the questionnaire was confirmed and its convergence validity was calculated to be 0.72. In addition, its internal consistency coefficient was 0.92 and its retest coefficient was 0.83 [36]. (Fig. 1)
3. RESULTS
The demographic variables of the two groups are presented in Table 2. According to the results of Chi-square test, there was no significant difference between the studied groups in terms of age, marital status, occupation, and level of education and they were homogeneous (p> 0.05).
The mean and standard deviation of depression and anxiety scores at pretest and posttest in both experimental and control groups are shown in Table 3. Multivariate analysis of variance results to compare experimental and control groups on dependent variables were also presented in Tables 4 and 5. In this study, multivariate analysis of covariance was used for the inferential analysis of the results. First, the required assumptions were examined. The assumptions of normality of distribution, homogeneity of variance, and equality of covariances were examined. The results of the Kolmogorov-Smirnov test showed that the distribution of data was normal (p> 0.05). Levene test results on the variables of depression (P = 0.669, F = 0.187) and anxiety (P = 0.988, F = 0.000) showed that the homogeneity of variance was confirmed for all variables of the study. Based on the Mbox test results (P = 0.467, F = 0.970, Mbox = 11.498), the equality of covariances were confirmed.
| Variable | Experimental, n(%) | Control, n(%) |
Value (Chi-Squared) |
P-value | |
|---|---|---|---|---|---|
| Age | 20 to 29 years | 5(33.33%) | 3(20%) | 1.58 | 0.45 |
| 30 to 39 years | 7(26%) | 6(40%) | |||
| 40 to 49 years | 3(20%) | 6(40%) | |||
| Status Marital | Single | 5(40%) | 3(20%) | 1.41 | 0.49 |
| Married | 4(26.66%) | 7(29%) | |||
| Divorce | 6(33.33%) | 5(33.33%) | |||
| Employment type | Employee | 4(26.665) | 5(33.33%) | 2.44 | 0.29 |
| Freelance Job | 3(20%) | 6(40%) | |||
| Homemaker | 8(32%) | 4(26.66%) | |||
| Education | Sub-Diploma | 5(33.33%) | 6(40%) | 1.41 | 0.41 |
| Diploma | 3(20%) | 5(33.33%) | |||
| Academic | 7(26%) | 4(26.66%) | |||
| Variables | Group | Pre-test | Post-test |
|---|---|---|---|
| Mean ± Std Deviation | Mean ± Std Deviation | ||
| Depression | experimental | 33.20±3.36 | 28.66±2.16 |
| Control | 35.00±2.26 | 35.53±2.64 | |
| Anxiety | experimental | 35.26±2.86 | 30.53±2.61 |
| Control | 36.60±2.38 | 35.66±2.19 |
| Test | Value | F |
Hypothesis df |
Error df |
P-value |
Partial Eta Squared |
Observed Power |
|---|---|---|---|---|---|---|---|
| Pillai’s Trace | 0.79 | 23.42 | 4 | 25 | .00 | 0.78 | 1 |
| Wilk’s Lambda | 0.21 | 23.42 | 4 | 25 | .00 | 0.78 | 1 |
| Hotelling’s Trace | 3.75 | 23.42 | 4 | 25 | .00 | 0.78 | 1 |
| Roy’s Larger Root | 3.75 | 23.42 | 4 | 25 | .00 | 0.78 | 1 |
|
Depended Variable |
Sum of Squares | df |
Mean Square |
F | P-value | Partial Eta Squared |
Observed Power |
|---|---|---|---|---|---|---|---|
| Depression | 353.63 | 1 | 546.13 | 60.77 | .00 | 0.68 | 1 |
| Anxiety | 197.63 | 1 | 276.03 | 33.93 | .00 | 0.54 | 1 |
As shown in Table 4, the value of Wilk’s lambda is significant (p <0.001). This means that there was a significant difference between the experimental and control groups in the posttest scores on the variables of depression and anxiety, and the difference was 0.78, i.e., 78% of individual differences in the variables were related to the differences between the groups.
According to the results of Table 5, by eliminating the effects of pretest scores, the difference between the mean of posttest scores in the variables of depression and anxiety in the experimental and control groups was significant (p<0.001). The effect of this treatment on reducing the score of depression was 68% and on reducing the score of anxiety was 54%.
4. DISCUSSION
This study aimed at evaluating the effectiveness of dialectical behavior therapy on depression and anxiety in Covid-19 patients after discharge from the hospital. The results showed that this treatment reduced the depression score of individuals. This finding was consistent with the findings of Harley et al. which evaluated the compatibility of dialectical behavior therapy skills training with refractory depression and showed that the experimental group significantly improved in reducing depressive symptoms compared to the control group [37]. Lynch et al. also aimed at evaluating the effectiveness of dialectical behavior therapy for depressed elderly people in a meta-analysis of twelve published studies, which showed that all 12 cases reported before and after depression treatment showed the effectiveness of dialectical behavior therapy on depression [38]. With the aim of comparing the effectiveness of Dialectical Behavior Therapy (DBT) and Compassion Focused Therapy (CFT) treatment in reducing depression and attempting suicide for borderline personality disorder, Lin et al. showed that they had similar reductions in depression and suicide after 6 months of intervention and follow-up. However, the effectiveness of DBT treatment was greater [39].
Dialectical behavior therapy leads to an increase in the level of consciousness along with a decrease in depressive symptoms, and according to theoretical foundations and research findings, there was an inverse relationship between general consciousness and depression. Dialectical behavior therapy increases anxiety tolerance along with reducing depression in individuals and leads to a reduction in depression [40]. Moreover, the most effective DBT strategies in treating depressive symptoms are considered components of tolerance for anxiety and pervasive consciousness. In general, DBT reduces the symptoms of depression by affecting the components of pervasive consciousness and anxiety tolerance [41].
The next finding showed the effects of dialectical behavior therapy on reducing anxiety scores. This finding was consistent with the research of Navarro-Haro et al., that found that both groups showed significant improvements in anxiety, depression, and emotion regulation problems. Tavakoli et al. showed that there was a significant improvement in the severity of the disorder after the intervention in both groups to compare dialectical behavior therapy and antianxiety medication on patients' anxiety and gastrointestinal symptoms. However, the greatest reduction in the severity of functional dysfunction was observed in the dialectical behavior therapy group compared to the other groups [42].
Aimand et al. investigated the effectiveness of DBT and Rational Emotive Behavior Therapy (REBT) in treating anxiety in male prisoners with antisocial personality disorder and showed that the DBT treatments affected all irrational beliefs and REBT only affected some beliefs. DBT was also more effective than REBT in treating anxiety in people with antisocial personality disorder [43]. Dialectical behavioral therapy helps patients learn ways to manage their conflicts. In fact, dialectical behavioral therapy with basic acceptance education teaches patients to accept life with problems and challenges and can reduce psychological damage such as anxiety by creating the ability to tolerate turmoil [44]. Moreover, dialectical behavior therapy using emotion regulation skills helps therapists to diagnose their feelings more accurately and then examine each emotion without being able to deal with it to ultimately reduce the person's anxiety. Thus, patients with Covid-19 can have more cognitive flexibility by using the dialectical behavior therapy method and have high efficiency in controlling their anxiety and in overcoming their negative emotions.
Limitations of this study included: 1. Low sample size used in this study 2. Not separating patients in terms of severity of the disease at the time of covid-19 (patients who were hospitalized in intensive care units or in general wards). 3. limitation was holding face-to-face training sessions for the experimental group, which, despite social distance and the use of personal protective equipment, still had the potential of infection with the Covid-19 virus, which is suggested to be considered in future research.
CONCLUSION
The findings of this study showed that dialectical behavior therapy can reduce anxiety and depression in patients with the Covid-19 virus. Therefore, to prevent further psychological consequences caused by this virus, it is recommended to use this intervention in designing treatment programs for psychological centers, comprehensive health service centers, counselors, clinical psychologists, and therapists.
LIST OF ABBREVIATIONS
| RCT | = Randomized Controlled Trial |
| BDI | = Beck Depression Inventory |
| BAI | = Beck Anxiety Inventory |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All procedures carried out in studies involving human participants were in accordance with the ethical committee No. IR.THUMS.REC.1400.001 approved by the Vice Chancellor for Research and Technology of Torbat Heydariyeh University of Medical Sciences.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used subset the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931). strict Institutional Animal Ethics Committee (IAEC) guidelines.
CONSENT FOR PUBLICATION
The necessary explanations were given to the individuals about the objectives of the research, and after obtaining informed consent, the individuals entered the project.
STANDARDS FOR REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this research are available from the corresponding author [A.G] upon request with permission from the Ethics Committee of Torbat Heydariyeh University of Medical Sciences.
FUNDING
None.
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank all relevant officials and all people for participating in this study.