All published articles of this journal are available on ScienceDirect.
Mapping Comorbidities Related to Autism Spectrum Disorder from Infancy to Adolescence: A Scoping Review
Abstract
Introduction
Children living with Autism Spectrum Disorder (ASD) often experience not only core ASD symptoms but also a range of comorbid biopsychosocial difficulties, including Attention-Deficit/Hyperactivity Disorder (ADHD), anxiety, epilepsy, sleep problems, and feeding or toileting challenges, each of which may contribute to developmental delays. This review aimed to systematically map and scope existing literature on comorbidities related to ASD from infancy to adolescence, identify the most common comorbidities, and delineate their characteristic symptoms and underlying aetiologies.
Methods
The researchers conducted a comprehensive search across academic databases – including MEDLINE, PsycINFO, Academic Search Premier, CINAHL, ScienceDirect, JSTOR Journals, EMBASE, and the Cochrane Library – accessed via platforms, such as EBSCOhost and ProQuest. Data from the 19 studies were analysed using Braun and Clarke’s six-phase framework for thematic analysis. A coding framework was collaboratively developed by the three authors, who independently reviewed and coded the data. Screening and data management were supported by the ASReview tool, and themes were refined through consensus to ensure analytical rigour and reliability.
Results
The review identified a spectrum of common ASD-related comorbidities that vary by developmental stage and context. Of an initial yield of 360 articles, 19 peer-reviewed studies met the inclusion criteria and were thematically analysed. Notably, studies from African settings were sparse, suggesting important regional research gaps.
Discussion
Cultural, environmental, and health factors influence the identification and prevalence of comorbidities associated with ASD. In clinical practice, our evaluation highlights the need for a comprehensive assessment protocol that takes into account the wide range of potential complications during different stages of development. Clinicians should recognize that symptoms can manifest differently at different ages and adapt their diagnosis and treatment methods accordingly.
Conclusion
Findings highlight the urgent need for culturally contextualised investigations of ASD comorbidities, particularly in underrepresented settings like sub-Saharan Africa. This review underscores the importance of developmental stage–sensitive diagnostic and treatment strategies.
1. INTRODUCTION
Autism Spectrum Disorder (ASD) is a lifelong neurodevelopmental disorder marked by social communication and interaction difficulties and repetitive behavioural patterns in interests or hobbies. Al-Beltagi [1] explains that ASD manifests on a spectrum that ranges from mild to severe, which may lead to challenging behaviour [1, 2]. Children who display symptoms of ASD may possess advanced language and cognitive abilities. Other children on the spectrum may have verbal and nonverbal impairments and may require lifelong care [3-5]. Children show comorbidities, which is indicative of the range of severity of symptoms of ASD [4]. ASD may be accurately identified in children as young as 24 months (two years). The mean age at which most children are diagnosed with ASD is between four and five years of age [1, 6]. Regardless of the increasing awareness and prevalence of ASD, the average age of ASD diagnosis has not changed [1, 7]. Additionally, signs of autism at this age relate to stage 3 of Erikson's psychosocial theory, as children with autism frequently show behavioural challenges both within and outside of the classroom, often rebelling and making poor choices. Many of the typical stages of psychosocial development are difficult for young people with ASD. This does not imply that only children living with autism display challenging behaviour; at this developmental stage, all children are more likely to show challenging behaviour.
Comorbid disorders are described as the presence of two or more disorders in the same individual, according to the American Psychiatric Association [8]. It is critical to be aware of comorbid disorders associated with ASD to accurately diagnose one condition as primary and the other as secondary [9, 10], to ensure that children with autism receive the appropriate care at different developmental stages. Mapping the different comorbid disorders provides an understanding of conditions that commonly co-occur with ASD in different psychosocial developmental stages. The prevalent ASD comorbidities that were mapped include toilet training difficulties, epilepsy, sleeping problems, feeding difficulties, eating disorders, ADHD, depression, and anxiety. The focus of this review was comorbidities, which are co-occurring behavioural challenges. The objectives of this scoping review were as follows:
i) To systematically scope the existing literature on the comorbidities related to ASD from infancy to adolescence
ii) To identify the common comorbidities of ASD in different psychosocial developmental stages
iii) To define specific characteristics – such as the symptoms and aetiology/causes of these comorbidities – in different psychosocial developmental stages.
To sharpen the analytical focus of this scoping review, we formulated the following guiding research questions:
1) What are the most commonly reported medical and psychiatric comorbidities associated with ASD from infancy through adolescence?
2) How do these comorbidities manifest across distinct psychosocial developmental stages as described in Erikson’s framework?
3) What gaps – geographical, methodological, or thematic – exist in the current literature on ASD comorbidities, particularly in underrepresented contexts, such as Africa?
1.1. Literature Review
This literature review explores the various comorbid disorders that manifest in children living with autism, particularly those that contribute to challenging behaviour during their developmental stages. This section draws on widely cited background literature to contextualise the aims of the review and is distinct from the findings derived from the scoping process. It meticulously maps these comorbid disorders against the psychosocial developmental stages to illuminate the intricate interplay between these disorders and developmental milestones. The review then delves into the specific intersections of psychosocial developmental stages and ASD, shedding light on the unique challenges and considerations within this context.
1.2. Comorbid Disorders for the Review Mapped against Psychosocial Developmental Stages
1.2.1. Toilet Difficulties
Toileting is a skill crucial for independent living. Individuals with autism face a significant barrier to quality of life when they struggle with this function [11]. A significant correlation has been established between low verbal ability, low cognition, and the age of accomplishment of bowel training in individuals living with autism [12]. This comorbidity shows that children living with ASD are more likely to feel ashamed and isolated when experiencing toilet difficulties. Twenty-two percent (22%) of autistic individuals between the ages of 9 and 32 still wet their beds [12]. Lower adaptive functioning is also associated with greater toileting difficulties [13]. A lack of research on toileting problems in ASD is evident [5]. Therefore, further research is needed in this area.
1.2.2. Seizures and Epilepsy
Epilepsy refers to a group of brain diseases in which a child experiences or is at risk of experiencing frequent and unexpected seizures as a result of abnormal electrical activity occurring in the brain [14, 15]. This abnormal electrical activity in the brain causes an individual to display abnormal movement or behaviour and feelings of odd sensations, which are referred to as convulsions or seizures [1]. When a child experiences a seizure, they will typically experience a brief period of unconsciousness, strange motion, body convulsions, or spells of staring [16]. Detecting epilepsy in children living with ASD may be challenging due to an overlap in symptoms [17], such as repetitive purposelessness in autism that resembles automatism in seizures, cognitive delays, impaired social interactions, and aggressive and irritable behaviour [18]. This indicates the need to identify the common comorbidities related to ASD in different psychosocial developmental stages as children grow. The care of a child who is experiencing seizures is more likely to be a challenge for both home-based caregivers and healthcare professionals who manage these comorbidities. Epilepsy is fairly prevalent, and 11-39% of children living with ASD have been reported to develop epilepsy [19]. Seizures commonly occur in children under five years of age and in adolescents [1]. Those who are more prone to epilepsy include children with moderate to severe intellectual disabilities, children who exhibit regression, and persons diagnosed with autism with additional neurological diseases [7]. Seizures and autism may potentially have a hereditary component [20].
1.2.3. Sleep Problems
Difficulties in falling and remaining asleep, sleepwalking, nightmares, and night terrors are the most prevalent sleep issues associated with children diagnosed with ASD [21]. Children living with ASD frequently experience sleep difficulties [22, 23]. Sleep problems are prevalent in 50-80% of children who have been diagnosed with ASD [24].
1.2.4. Eating Disorders
Eating disorders are severe mental illnesses that have a negative impact on physical health [25]. The most common eating disorders are anorexia nervosa, bulimia nervosa, binge eating disorder, and avoidant restrictive food intake disorder. Children living with ASD frequently exhibit unusual eating behaviours [26]. These behaviours include avoiding certain foods, consuming non-food things, and picking at food without swallowing [26]. They also include sensory sensitivity to specific foods. Individuals who have these eating disorders have a higher susceptibility to being diagnosed with autism than those who do not have eating disorders [27]. There is little information available on how many people living with autism have eating disorders [17].
1.2.5. Attention-Deficit/Hyperactivity Disorder (ADHD)
Many children experience difficulties with sitting still, impulse control, and maintaining concentration. However, in children living with attention-deficit hyperactivity disorder (ADHD), these behaviours can be excessive and significantly impact their daily functioning [28]. While some children primarily exhibit inattentive symptoms, it is common for these behaviours to co-occur with hyperactivity and impulsivity [29]. Notably, there is an overlap in the symptomatic presentation of ASD and ADHD. For instance, both conditions may manifest as apparent inattentiveness during conversations, frequent interruptions, or disregard for personal space [30]. Indeed, a substantial proportion of children with ASD display symptoms that closely resemble those of ADHD [1].
1.2.6. Depression
High-functioning children living with ASD may be more susceptible to depression than their lower-functioning counterparts due to their enhanced social and self-awareness, coupled with a heightened interest in social relationships [6]. The discrepancies in social circumstances and relationships, as well as the experience of being misunderstood or rejected by neurotypical individuals, can contribute significantly to anxiety and stress [31]. These factors may lead to low self-esteem, social isolation, and loneliness, all of which can precipitate depression [20].
Depressive symptoms typically manifest as a decline in mood, disrupted sleep and appetite patterns, increased irritability, and a lack of motivation [32]. It is worth noting that, in children, depressive symptoms may present as irritability rather than overt sadness or negative emotions [32]. Depression is particularly prevalent among children with ASD who are cognisant of their social challenges. Furthermore, children with ASD may be at a higher risk of experiencing depressive symptoms if they exhibit more severe autism symptoms, are older, and possess a higher verbal IQ [31].
1.2.7. Anxiety
Anxiety disorders are prevalent among individuals with ASD, affecting both children and adults [20, 33]. Factors, such as age, cognitive performance, social impairment, and ASD-specific issues, can significantly influence the manifestation of anxiety symptoms [33]. Various forms of anxiety disorders, including generalised anxiety disorder and social anxiety disorder, are often underdiagnosed in individuals with ASD because these symptoms are frequently attributed to ASD itself. Consequently, distinguishing whether symptoms like compulsive checking are part of ASD or a co-occurring anxiety disorder can be challenging [34]. Empirical studies, such as the one conducted by White et al. [35], have critically examined the overlapping and distinct aspects of anxiety as a comorbidity of ASD.
Individuals with anxiety may experience symptoms, such as tension, restlessness, hyperactivity, worry, and fear [36]. Children with high-functioning ASD scored higher on measures of total anxiety, social anxiety disorder, and panic disorder, compared to a control group of children without an ASD diagnosis [37]. Additionally, a meta-analysis reported a 39.6% prevalence of at least one anxiety disorder among children with ASD [38]. Social anxiety is particularly common, as children with autism often face social challenges that can lead to feelings of tension and discomfort [31]. Anxiety in children with autism can manifest in various ways, including increased stimming, repetitive questioning, self-injury, and sleep disturbances [36].
The developmental trajectory of anxiety in individuals diagnosed with ASD shows a rise during the toddler years, peaking in childhood, decreasing during young adulthood, and increasing again in older age [5, 7, 39-41]. Building on this understanding of anxiety's fluctuating presence across the lifespan of individuals with ASD, our review next turns to a comprehensive analysis of how these patterns intersect with, and are influenced by, psychosocial developmental stages in ASD.
While the focus of this review remains on established clinical and psychosocial comorbidities of ASD, it is also important to acknowledge the growing body of research employing predictive and data-driven methodologies for behavioural insight. Recent studies from fields, such as digital marketing and virtual environments, have explored the use of text mining and machine learning to analyse unstructured behavioural data. For example, Izumi et al. applied text mining techniques to post-purchase customer feedback to infer behavioural trends, while Prasetio et al. used advanced machine-learning methods for behavioural detection in metaverse platforms [42, 43]. Although these studies were not conducted in clinical contexts, the analytical techniques they demonstrate may offer future potential for tracking ASD-related comorbidities over time and across settings.
1.3. Psychosocial Developmental Stages and ASD
1.3.1. Infant Autism: Behavioural Characteristics
Typically, signs of ASD become apparent in infants between 12 and 24 months of age [44]. However, the Autism Science Foundation notes that some infants can exhibit signs of autism as early as 2 months old [44, 45]. Autism does not alter a baby's physical appearance but significantly affects their communication and interaction with the world around them [46, 47]. Key behavioural indicators include reduced eye contact [48], minimal gesturing [49], limited response to their name [50], delayed language or speech development [51], diminished emotional expression in facial gestures [52], and regression of previously acquired skills [53].
One and two-year-old children with ASD often exhibit early signs of social isolation [33]. While typically developing eighteen-month-old children usually show a strong interest in social interactions, toddlers with autism tend to prefer isolation [7]. Recent research suggests that early brain imaging may offer promising potential for the presymptomatic prediction of ASD [54]. This study supports the consensus that earlier interventions can lead to more successful outcomes for the child.
1.3.2. Autism in Childhood
An autism diagnosis is most commonly made between the ages of three and four years, when behavioural deficits and excesses are well defined [7]. The behavioural development of an autistic child can be categorised into three primary areas: (i) socialisation, (ii) communication, and (iii) play/imagination.
1.3.3. Autism in Adolescence
ASD symptoms can evolve from childhood to adulthood [55]. In many cases, autism cannot be diagnosed unless its symptoms are evident during early childhood, allowing for the establishment of a behavioural pattern [56-58]. There is no specific age at which these indicators of autism appear in teenagers. However, as with many adolescents, behavioural and emotional changes may become noticeable as they reach puberty, typically between the ages of 9 and 14 years [59]. Autism symptoms may also become more pronounced as teenagers enter middle and high school, where social relationships often gain greater importance [17, 60]. Additionally, adolescence can be particularly stressful for autistic individuals. Despite experiencing the same hormonal changes as their peers, autistic teenagers do not naturally form complex relationships and often struggle to interpret or engage in the various types of interactions that emerge as they grow older [33]. They are prone to solitude and low moods, which can manifest as intense and difficult-to-read emotions [61].
2. METHOD
The process of conducting a scoping review is deemed less prescriptive than that of, for example, a systematic literature review. Nevertheless, some guidelines, as determined by [62], have been adopted as a yardstick for conducting a scoping review. Background literature cited in the introduction was not considered part of the formal scoping review dataset.
2.1. Search Strategy
The search strategy was designed to be both comprehensive and methodologically rigorous in order to address the review’s objectives effectively. A systematic electronic search was conducted across the following academic databases: MEDLINE, APA PsycINFO, Academic Search Premier, CINAHL with Full Text, ScienceDirect, JSTOR Journals, EMBASE, and the Cochrane Library. Additional sources included Springer Nature Journals, Scopus, SciELO, and Health Source: Nursing/Academic Edition. These databases were accessed through multiple platforms, including EBSCOhost, ProQuest, and individual publisher portals. All searches were executed using the EBSCO Discovery Service in close coordination with a qualified subject librarian and a student research psychologist, both of whom contributed to feasibility testing, search term refinement, and the selection of database sources to ensure methodological accuracy and efficiency.
The search was limited to a 15-year publication window (2007–2022) to capture contemporary, peer-reviewed studies published during a period of heightened diagnostic standardisation and evolving clinical frameworks, particularly following the introduction and adoption of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria [8] in 2013. This time frame also corresponds with a critical era in autism research, marked by increased attention to comorbidities, improved diagnostic tools, and more sophisticated methodologies for studying co-occurring developmental and psychiatric conditions.
The Boolean keyword string used for the search was as follows: (“comorbidities” OR “comorbidity” OR “comorbid disorders”) AND (“autism spectrum disorders” OR “autism” OR “ASD” OR “psychosocial developmental stages”) AND (“review” OR “scoping review”).
As appropriate, these terms were searched within titles, abstracts, and subject headings (e.g., MeSH and EMTREE). Results were restricted to peer-reviewed academic journal articles.
This scoping review was not pre-registered in the International Prospective Register of Systematic Reviews (PROSPERO) or the Open Science Framework (OSF). While registration is encouraged to enhance methodological transparency, it is not a formal requirement under the Arksey and O’Malley framework [62], or PRISMA-ScR guidelines for scoping reviews [63].
2.2. Inclusion and Exclusion Criteria
2.2.1. Inclusion
Articles were included if the study population comprised infants to adolescents (1-19 years old) and if the focus was on comorbidities related to autism spectrum disorder. Academic articles were included because they were peer-reviewed and generally of a high academic standard. All methods and approaches were included so that co-occurring behavioural challenges could be mapped. Articles had to be written in English.
2.2.2. Exclusion
Any studies that did not correspond with the proposed study definition criteria were excluded from the research. The format of these studies was different from that of peer-reviewed academic or scientific articles, and, as such, most books and book chapters, as well as editorials, review letters, posters, meetings, abstracts, and proceedings were excluded.
2.3. Study Screening
After all the results had been compiled, duplicates were removed. The remaining articles were screened in duplicate by the review team (A.M, W.T, and C.M). To support this process, ASReview – an open-source, AI-assisted screening tool – was used during the title and abstract phase to help prioritise and organise articles based on predicted relevance to the inclusion criteria. Screening was first conducted according to title and abstract using the designed inclusion and exclusion criteria. The full texts of all articles that met the criteria were independently screened by the review team (A.M, W.T, and C.M). Any disagreements during the screening process were discussed during a Microsoft Teams meeting until consensus was reached.
As this was a scoping review rather than a systematic review, we did not conduct a formal methodological quality appraisal of the included studies. This decision aligns with established scoping review frameworks. According to Arksey and O’Malley [62] and the PRISMA-ScR guidelines [62], the primary aim of a scoping review is to map the extent, range, and nature of available research rather than to evaluate the quality of individual studies. Levac et al. [43] further clarify that, while critical appraisal may be incorporated when relevant, it is not a standard or required component of scoping reviews unless the research objective specifically includes assessing the robustness of evidence. Similarly, the JBI guidance for scoping reviews [63, 64] emphasises that study quality appraisal is not mandatory and is generally omitted unless justified by the review’s purpose. Accordingly, our focus remained on providing a broad thematic overview of ASD-related comorbidities across developmental stages, consistent with the goals of a scoping methodology.
2.4. Data Extraction
All articles that met the full-text criteria were included for data extraction. Results were reported according to the objectives of the review. A data chart was created of authors and year, title, setting, design/approach, and findings. Data extraction was conducted in duplicate with three reviewers independently extracting data from all studies included. To ensure rigor and accuracy, the review team extracted data independently, and the results were compared. Any discrepancies were discussed to ensure consistency between the reviewers. The findings would be disseminated in different ways, such as publication in a peer-reviewed journal and other key system stakeholders (Department of Health in South Africa), and presentations at conferences.
3. RESULTS
The findings section delves into the intricate landscape of comorbid conditions in ASD across various developmental stages. These results are based solely on the 19 studies that complied with the inclusion criteria; none of the background literature cited in the introduction is repeated. It unfolds through three pivotal themes: the emergence of comorbidity in infants with ASD, the array of comorbid conditions in children with ASD, and the evolving nature of these conditions in adolescence. These themes reveal the complex interplay between comorbid conditions and developmental growth in individuals with ASD.
Figure 1 presents the flow of the study selection process for this scoping review on comorbidities linked to ASD across psychosocial developmental stages. A total of 360 records were identified through database searches. During the initial title and abstract screening phase, 323 records were excluded. Most of these did not clearly focus on comorbidities related to ASD, included age groups outside infancy to adolescence, or did not appear to be of academic standard. After this stage, 37 full-text articles were reviewed for eligibility. Of these, 18 were excluded following closer inspection due to confirmed reasons, such as age ineligibility or lack of focus on comorbidities. This process resulted in the inclusion of 19 studies in the final synthesis.
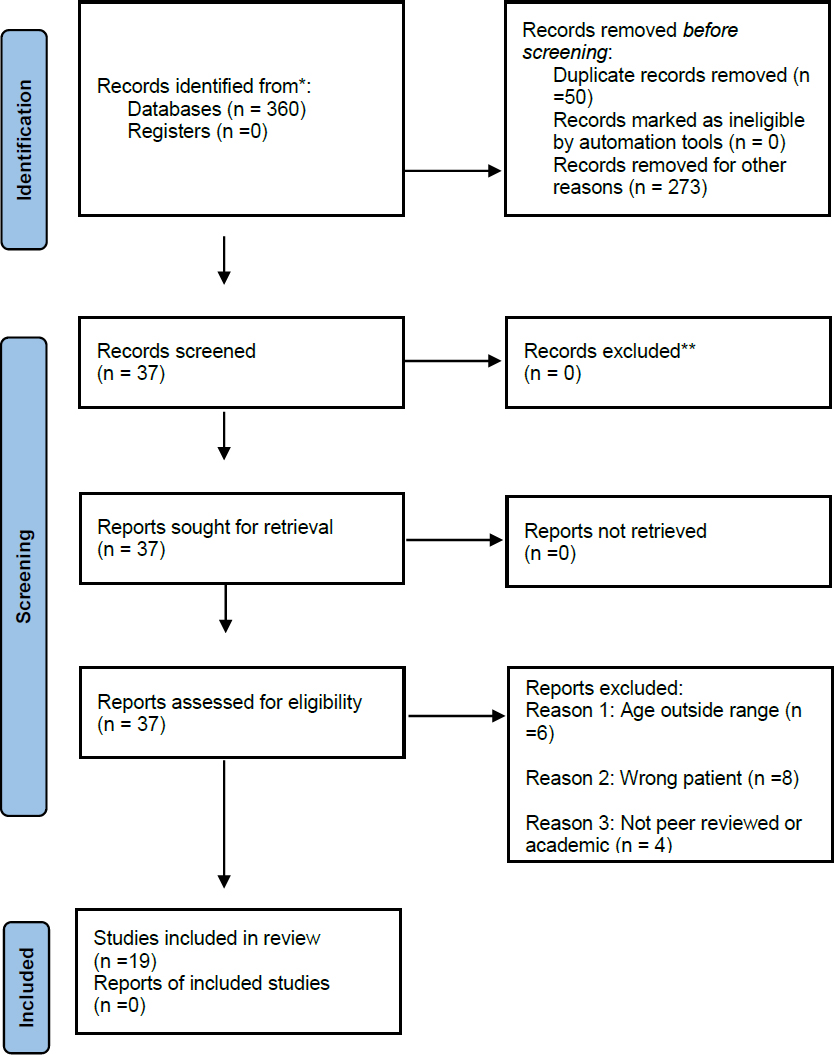
PRISMA flow diagram outlining the study selection process.
| S.No. | Comorbidity | Infancy/Toddlerhood | Childhood | Adolescence | Prevalence Range (if reported) | No. of Studies |
|---|---|---|---|---|---|---|
| 1. | ADHD | √ | √ | √ | 31 – 84% | 6 |
| 2. | Anxiety | √ | √ | √ | 20 – 58% | 9 |
| 3. | Epilepsy | √ | √ | √ | 11 – 73% | 5 |
| 4. | Sleep problems | √ | √ | √ | 50 – 91% | 4 |
| 5. | Gastrointestinal issues | X | √ | √ | 84.4% | 2 |
| 6. | Depression | X | √ | √ | 13 – 36% | 5 |
| 7. | Toileting issues | √ | √ | X | Unknown | 2 |
| 8. | Feeding/eating disorders | √ | √ | √ | Varied | 3 |
| 9. | Intellectual disability | √ | √ | √ | 46 – 76% | 3 |
| 10. | Mood disorders | X | √ | √ | 36.4% | 2 |
3.1. Publication Location
This scoping review sampled peer-reviewed journal articles through a Boolean search, resulting in the identification, inclusion, and analysis of 19 articles, as tabulated in Table 1. Of these, 11 were published in the United States of America (Davis et al., 2011; Davis et al., 2012; Fodstad et al., 2010; Hess et al., 2010; Jahromi et al., 2013; Joshi et al., 2010; Kozlowski et al., 2012; Leyfer et al., 2006; Ming et al., 2008; Moseley et al., 2011; and Strang et al., 2012). Two articles were published in Ireland (Mannion et al., 2013 and Mannion et al., 2016), one in Saudi Arabia (Amr et al., 2012), one in South Africa (Pillai et al., 2021), one in Nigeria (Bakare et al., 2019), one in the Democratic Republic of the Congo (Mpaka et al., 2016), one in Japan (Munesue et al., 2008), and one in England (Simonoff et al., 2008).
3.2. Thematic Analysis
Themes were identified and analysed thematically. We used Braun and Clarke’s six-phase approach to thematic analysis [65] to engage with both the identified themes (comorbid conditions in infants, children, and adolescents living with an autism spectrum disorder) and the relevant literature.
Firstly, we read and extracted data to familiarise ourselves with the data. Secondly, we organised data systematically by developing codes in MS Teams meetings to ensure that there was no bias. Thirdly, we generated themes to address the aim of the review, and fourthly, we read the identified themes that were aligned with the aim of the study.
3.3. Comorbid Conditions in Infants Living with an Autism Spectrum Disorder
Previous studies [39-41, 66] found that toddlers living with ASD experience more severe comorbid symptoms than both typically developing toddlers and those with other developmental delays. This implies that toddlers require particular care to minimise challenging behaviour once they reach adolescence. The comorbid symptoms identified in this study include conduct disorder/tantrums, anxiety, impulsiveness, inattention, avoidance behaviour, eating problems, and sleeping problems. The same study reported that – apart from avoidance behaviour, eating problems, and sleeping problems that remained consistent across all age groups – the classes of comorbid behaviour became increasingly severe amongst older age groupings (12–18 months, 19–24 months, 25–31 months, 32–39 months) of toddlers living with ASD. While both typically developing (neurotypical) and atypically developing children may exhibit challenging behaviours at similar ages, such behaviours are often more frequent and pronounced among children with ASD.
A range of ASD symptom profiles and severity levels was investigated by [13, 67, 68], who found that toddlers living with ASD presented with significantly more feeding and sleeping problems than atypically developing toddlers and toddlers living with Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS). In support of the previous study [39, 68], it was found that toddlers living with ASD reported significantly higher anxiety and avoidance scores than atypically developing toddlers and toddlers living with PDD-NOS. This means that caregivers will struggle to notice or identify problematic behaviour in a child until they are diagnosed by a professionally qualified healthcare practitioner (occupational therapist, pediatrician, psychiatrist, or psychologist).
Davis et al. (2011) expanded on the previous study [39] and found that ASD toddlers with higher communication scores presented with higher anxiety scores. The authors of this study further discussed the significance of communication on the anxiety experienced by toddlers living with autism spectrum disorders and how their communication relates to their understanding of what to be anxious about. Additionally, females reported significantly higher communication scores.
3.4. Comorbid Conditions in Children Living with an Autism Spectrum Disorder
A study [69] explored differences in self-regulation among 20 children diagnosed with ASD and 20 typically developing children (without any diagnosis) throughout the schooling year. Children diagnosed with ASD showed significantly less emotional regulation and control, cooperative and independent class participation, and prosocial peer engagement than their typical developing peers [69]. For instance, when they are attending a mainstream school, they are more likely to struggle to build social relations and class engagement. Additional studies correspond with the findings asserting that children diagnosed with ASD have substantial difficulties with active classroom engagement, emotional regulation, social connectedness, initiating communication, classroom participation, and flexibility [70, 71]. Therefore, teachers in mainstream schools must be trained to cater to children living with ASD. Practically, children living with ASD require special needs schools that accommodate children with ASD.
The co-occurrence of medical and psychiatric comorbidities in children living with Asperger's syndrome and children living with PDD was investigated [72]. The authors of this study found that sleep disorders were the most common comorbid condition amongst children living with autism, gastrointestinal dysfunction was the most common amongst children living with PDD, and mood disorders comprised the most common comorbidity amongst children living with Asperger's syndrome. These results show that children living with ASD are more likely to be diagnosed with two or more disorders. This is a cause for concern for caregivers and biopsychosocial healthcare practitioners because it is more likely to complicate caring for these children.
Another study [73] discovered that children and adolescents living with ASD and typically developing children display different symptoms of worry, depressed behaviour, under-eating, repetitive behaviour, and avoidant behaviour. However, no significant differences in conduct were found between children and adolescents living with ASD and typically developing children.
A study by Davis et al. (2010) [40] compared communication scores and anxiety symptoms of children living with ASD and PDD-NOS with those of children with no diagnosis. An increase in communication deficits was associated with a decrease in anxiety for the group of children living with ASD compared to children living with PDD-NOS and undiagnosed children. Moreover, a study by [74] found that youth diagnosed with ASD suffered from significantly more comorbid psychiatric conditions than youth without ASD. Anxiety disorders, including agoraphobia, were much more prevalent in youth diagnosed with ASD, while youth without ASD had a much higher prevalence of substance abuse disorders [74]. In addition, social anxiety disorder was found to be the most common comorbidity, followed by ADHD and oppositional defiant disorder (ODD).
The most common comorbidity among children diagnosed with ASD was specific phobias, followed by obsessive-compulsive disorder [75]. A similar study [76] identified the types and rates of psychiatric comorbidities in children diagnosed with ASD. These findings are consistent with other studies [77-79]. Additionally, a study [76] found that 70% of children with ASD had a minimum of 1 comorbidity and 41% had 2 or more comorbidities. In support, another study found that 63% of children were diagnosed with a minimum of 1 comorbid psychiatric disorder [80]. Psychiatric symptoms of anxiety and depression in children living with ASD were examined by Strang et al. [81], who found that 56% of the children were in the clinical range of anxiety symptoms and 24% of children fell into the borderline range of depression. These statistics indicate that there must be an awareness of the rate of comorbidities to assist society and biopsychosocial healthcare practitioners in providing care.
A sub-Saharan African study by Mpaka et al. [82] found intellectual disability/cognitive disorders (75.83%) and epilepsy (72.50%) to be the most common comorbidities in a sample of 120 children living with ASD. This implies that there is a high rate of children living with ASD who require care. Additionally, 93.33% of the ASD-diagnosed samples were diagnosed with 1 to 4 comorbidities, while 6.67% of the children diagnosed with ASD were without comorbidities. Unfortunately, these results signify an increase, and it is worrisome that children living with ASD are likely not to receive special care due to a lack of resources (hospitals, schools, and healthcare centres) or little to no human resources that specialise in ASD. The same study found a positive relationship between the number of comorbidities and the age of children, with high numbers of comorbidities being much more prevalent in older children diagnosed with ASD [82].
These findings were supported by another African study [83, 84] conducted in Nigeria. Bakare et al. (2019) [83] found that comorbid intellectual disability was prevalent amongst half of the children diagnosed with ASD in the Nigerian cohort studies [85, 86]. Additionally, another Nigerian study conducted [84] found that ADHD and epilepsy/seizure disorder were frequently occurring comorbidities in Nigerian children diagnosed with ASD throughout their scoping review.
A South African study [2] found that ADHD was the most common comorbidity (43%) in children diagnosed with ASD in Kwa-Zulu Natal, followed by intellectual impairment (17%) and epilepsy (15%). Notably, this South African study reaffirms much of the existing literature on comorbid conditions internationally associated with children living with ASD, namely, seizures/epilepsy, sleep disturbances, behavioural challenges, gastrointestinal disturbances, learning disorders, and anxiety.
3.5. Comorbid Conditions in Adolescents Living with an Autism Spectrum Disorder
A study examined comorbid psychopathology in children and adolescents with ASD and found that 46.1% of participants had a comorbid disorder, and 15.7% presented with an anxiety disorder [5]. Intellectually disabled children diagnosed with ASD had an increased likelihood (78.7%) of being diagnosed with a comorbid disorder. This study further found that under-eating and avoidant behaviours were significant predictors of sleep problems in children and adolescents diagnosed with ASD. Following up on a study by Mannion et al. [5], a study [4] assessed whether the comorbid symptoms identified in the initial study had changed over a two-year period. The follow-up study found that sleep problems persisted among 91.5% of past participants, gastrointestinal problems persisted among 84.4% of past participants, and eating problems became increasingly severe among participants [4]. These results indicate that adolescents are no different from children living with ASD. Additionally, the lack of specialised healthcare for these children means that they are likely to experience the same challenges once they reach adolescence.
A Japanese study [87], found that 36% of adolescents were diagnosed with a mood disorder, with bipolar disorder accounting for 75% of the cases. For most individuals diagnosed with ASD, these comorbid mood disorders occurred in late adolescence. Notably, among the three ASD subcategories in this study (AD, Asperger disorder, and PDD-NOS), no adolescents diagnosed with autistic disorder (AD) received comorbid diagnoses of mood disorders.
Types and rates of comorbid mental disorders in adolescents diagnosed with autism were investigated by Moseley et al. (2011) [43, 88]. Of the 84 adolescents sampled, the authors found that 42% of those living with autism were diagnosed with a comorbid mental disorder, a rate two to four times higher than that of typically developing adolescents. Comorbidities identified in this study included mood disorders (17%), disruptive behaviour disorders (12%), anxiety disorders (12%), and adjustment disorders (8%).
4. DISCUSSION
4.1. Review Objectives and Key Findings
This scoping review aimed to systematically examine the existing literature on comorbidities related to ASD from infancy to adolescence, identify common comorbidities across different psychosocial developmental stages, and define specific characteristics, such as symptoms and aetiology of these comorbidities. Our analysis of 19 articles revealed several key findings that address these objectives.
4.2. Systematic Scoping of Existing Literature
Our scoping review not only confirmed the widely recognised gap in literature regarding comorbid conditions in infants with ASD [5, 39, 40, 66, 89] but also provided a comprehensive mapping of comorbidities across different developmental stages. This mapping revealed a notable progression and evolution of comorbidities from infancy through adolescence, a perspective not previously synthesised in the literature.
While the majority of studies in our review focused on childhood and adolescence, our analysis uniquely juxtaposed findings across all developmental stages. This approach allowed us to identify key transitions and changes in comorbidity patterns that occur as individuals with ASD age. For instance, we found that certain comorbidities, such as anxiety, persist across stages but manifest differently, while others emerge or become more prominent in specific developmental periods.
This comprehensive view not only highlights the need for more research on early identification and intervention strategies but also emphasises the importance of a developmental approach to understanding and treating ASD-related comorbidities. Our findings suggest that interventions may need to be tailored not just to the specific comorbidity, but also to the developmental stage of the individual with ASD.
4.3. Common Comorbidities Across Psychosocial Developmental Stages
Our review identified two overarching themes of comorbidities across all psychosocial developmental stages: medical and psychiatric. This finding suggests that ASD-related comorbidities are not limited to a single domain but span across various aspects of an individual's health and well-being.
In infancy and toddlerhood, common comorbidities included conduct disorders, anxiety, impulsivity, and sleep problems [39, 66]. Interestingly, the severity of these comorbidities appeared to increase with age, even within this early developmental stage.
During childhood, the range of comorbidities expanded to include emotional regulation difficulties, social engagement issues, and various anxiety disorders [69, 74]. These findings highlight the increasing complexity of comorbidities as children with ASD enter school and face new social and academic challenges.
In adolescence, anxiety disorders remained prevalent, with the addition of mood disorders and adjustment difficulties [5, 87]. This progression suggests that, while some comorbidities persist across developmental stages, new challenges emerge as individuals with ASD navigate the complexities of adolescence.
To improve clarity and cross-comparative interpretation, Table 2 summarises the comorbidities reported across developmental stages, along with their prevalence ranges (where available) and the number of studies in which each comorbidity was observed.
4.4. Specific Characteristics of Comorbidities
The review revealed that the manifestation and severity of comorbidities can vary based on the specific ASD diagnosis. For instance, toddlers with autistic disorder experienced more severe anxiety and avoidant behaviours compared to those with other ASD diagnoses [39]. This finding underscores the importance of considering the specific ASD diagnosis when assessing and treating comorbidities.
Our analysis also highlighted geographical differences in reported comorbidities. Studies from African countries reported higher rates of intellectual impairment, cognitive disorders, and epilepsy compared to Western studies [2, 82, 83]. This discrepancy raises important questions about the role of cultural, environmental, and healthcare factors in the identification and prevalence of ASD-related comorbidities.
| Authors and Year | Title | Setting | Design/approach | Findings |
|---|---|---|---|---|
| 1. Amr et al. (2012) [80] | Comorbid psychiatric disorders in Arab children with autism spectrum disorders. | Saudi Arabia | Mixed method approach; Clinical interview and a semi-structured clinical interview |
Sixty-three percent of the children were diagnosed with at least one comorbid disorder. The most commonly reported comorbid disorders were found to be anxiety disorders (58.3%), ADHD (31.6%), conduct disorders (23.3%), and major depressive disorder (13.3%). |
| 2. Bakare et al. (2019) [84] | Autism Spectrum Disorders in Nigeria: A scoping review of literature and opinion on future research and social policy directions | Nigeria | Review study; Scoping review |
This study was a scoping review of ASD in Nigeria with the goal of offering expert opinions on possible future research and social policy directions in the country. |
| 3. Davis et al. (2011) [39] | Anxiety symptoms across the lifespan of people diagnosed with autistic disorder | United States of America | Observational study design; The Baby and Infant Screen for Children with aUtIsm Traits – Part 2 (BISCUIT-Part 2) and Autism Spectrum Disorders – Comorbidity for Children (ASD-CC) |
Results indicated that there is a significant difference between different age cohorts on symptom endorsements of anxiety |
| 4. Davis et al. (2012) [41] | The effect of communication deficits on anxiety symptoms in infants and toddlers with autism spectrum disorders | United States of America | Quantitative research design BDI-II Baby and Infant Scale for Children With aUtIsm Traits Part 2 (BISCUIT-Part 2) |
Both receptive and expressive communication skills appeared to play a significant role in the manifestation of anxiety symptoms in children with ASD. |
| 5. Fodstad et al. (2010) [66] | Emergent Comorbidity in At Risk Children with and without Autism Spectrum Disorder-A Cross-Sectional Study. | United States of America | Observational research design; Interviews with parents/legal guardians |
A general trend emerged where toddlers living with ASD appeared to have more severe symptoms than atypically developing non-ASD toddlers, with an increasing trend of comorbid behaviour as they grow older. |
| 6. Hess et al. (2010) [73] | Psychiatric Symptom Endorsements in Children and Adolescents Diagnosed with Autism Spectrum Disorders: A Comparison of Typically Developing Children and Adolescents | United States of America | Quantitative research design; A 19-item composite symptom checklist from the DSM-IV-TR (APA, 2000) and the International Classification of Diseases, Tenth Edition (ICD-10; World Health Organization, 1992) was used to assess all participants. |
The subscales of the ASD-CC – worry/ depressed, under-eating, over-eating, avoidant behaviour, and repetitive behaviour – all contribute to the significant difference between groups. |
| 7. Jahromi et al. (2013) [69] | The importance of self-regulation in school and peer engagement of children with high-functioning autism | United States of America | Qualitative research design; Questionnaires |
Children with high functioning autism (HFA) had significantly impaired self-regulation and decreased school and peer engagement. |
| 8. Joshi et al. (2010) [74] | The Heavy Burden of Psychiatric Comorbidity in Youth with Autism Spectrum Disorders: A Large Comparative Study of a Psychiatrically Referred Population | United States of America | Quantitative research design; The K-SADS-E semi structured interview that generates current and lifetime Axis-I diagnoses according to DSM-III-R/IV criteria in children and adolescents. |
ASD youth suffer from a significantly higher number of comorbid disorders than comparisons. 95% of the youth with ASD had three or more comorbid psychiatric disorders and 74% had five or more comorbid disorders. |
| 9. Kozlowski et al. (2012) [67] | Feeding and sleep difficulties in toddlers with autism spectrum disorders | United states of America | Quantitative research design; A comprehensive battery of assessments and interviews with parents/legal guardians. |
Individuals with Autistic Disorder were found to exhibit significantly more feeding and sleep difficulties than those with PDD-NOS, who in turn presented with more difficulties of this type than those with atypical development. |
| 10. Leyfer et al. (2006) [75] | Comorbid Psychiatric Disorders in Children with Autism: Interview Development and Rates of Disorders. | United States of America | Qualitative Research design; The Autism Comorbidity Interview Present and Lifetime Version (ACI-PL). |
This study confirmed the frequent co-occurrence of autism with other psychiatric disorders. Seventy-two percent of the children in this study had at least one DSM-IV Axis I psychiatric disorder in addition to autism. |
| 11. Mannion & Leader (2016) [5] | An investigation of comorbid psychological disorders, sleep problems, gastrointestinal symptoms, and epilepsy in children and adolescents with autism spectrum disorder: A two-year follow-up. | Ireland | Quantitative research design; Questionnaires (Children’s Sleep Habits Questionnaire; Autoimmune Disease in Family Members Questionnaire) and scales (Autism Spectrum Disorder-Comorbid for Children [ASD-CC]). |
Sleep problems persisted in 91.5% of participants. Gastrointestinal symptoms persisted in 84.4% of participants. There was a significant difference between at baseline and at two-year follow-up from Mannion et al. (2013), where overeating became more severe over time. It was found that 92.9% of participants presented with a family history of autoimmune disease. |
| 12. Mannion et al. (2013) [5] | An investigation of comorbid psychological disorders, sleep problems, gastrointestinal symptoms, and epilepsy in children and adolescents with Autism Spectrum Disorder. | Ireland | Quantitative research design; Informant survey |
The prevalence of a comorbid disorder was 46.1% (n=41). This rate increased to 78.7% when intellectual disability was included as a comorbid disorder. |
| 13. Ming et al. (2008) [72] | Autism spectrum disorders: concurrent clinical disorders. | United States of America | Mixed methods research design; Clinical intake forms completed by parents and medical history |
Medical co-occurrence did not present as a risk factor for psychiatric co-occurrence, and vice versa. Results showed a high prevalence of multiple medical and psychiatric co-occurrences in children diagnosed with ASD. |
| 14. Moseley et al. (2011) [88] | Psychiatric comorbidities in adolescents and young adults with autism | United States of America | Quantitative research design; A semi-structured comprehensive clinical interview with all participants and caregivers and supplemented by quantitative questionnaires. |
42% of the young people living with autism in the sample had an additional comorbid mental disorder |
| 15. Mpaka et al. (2016) [82] | Prevalence and comorbidities of autism among children referred to outpatient clinics for neurodevelopmental disorders | Democratic Republic of the Congo | Mixed method research design; Extensive clinical interview and observation and intellectual quotient evaluation and electroencephalogram reporting. |
Of the 450 subjects referred, 120 (29.3%) received the diagnosis of ASD, with boys outnumbering girls (OR 3:1). Intellectual disability (75.83%) and epilepsy (72.50%) were the main comorbidities significantly associated with autism. |
| 16. Munesue et al. (2008) [87] | High prevalence of bipolar disorder comorbidity in adolescents and young adults with high-functioning autism spectrum disorder: A preliminary study of 44 outpatients. | Japan | Quantitative research design; Retrospective study |
Sixteen patients (36.4%) were diagnosed with a mood disorder. |
| 17. Pillai et al. (2021) [2] | A study reflecting the demographics and comorbidities of children diagnosed with autism spectrum disorder at initial presentation to the KwaZulu-Natal Children’s Hospital | South Africa | Quantitative research design Retrospective review |
ADHD was the most common comorbidity, affecting 43% of participants. |
| 18. Simonoff et al. (2008) [76] | Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-driven sample | England | Quantitative Research design; The Child and Adolescent Psychiatric Assessment-Parent Version (CAPA). |
The most common diagnoses were social anxiety disorder, ADHD, and oppositional defiant disorder. Of those with ADHD, 84% received a second comorbid diagnosis. |
| 19. Strang et al. (2012) [81] | Depression and anxiety symptoms in children and adolescents with autism spectrum disorders without intellectual disability | United States of America | Quantitative research design; Child Behavior Checklist (CBCL), WISC-IV, and the WASI subtests. |
These findings indicate an increased risk for depression/anxiety symptoms in children and adolescents with ASDs without intellectual disability, regardless of age, IQ, or ASD symptoms. |
Future research may benefit from interdisciplinary methodologies that extend beyond traditional thematic synthesis or clinical case analysis. Predictive tools, such as machine-learning algorithms, text mining of electronic health records, or behavioural signal extraction from unstructured data, could enable earlier and more precise detection of ASD-related comorbidities. Adapting such methodologies to ASD research could transform the way comorbidity risk is predicted, visualised, and managed across developmental stages.
5. STRENGTHS AND LIMITATIONS
A key strength of this scoping review is the rigorous and ethical approach taken to data extraction and interpretation. The reviewers ensured that data were extracted fairly, honestly, and without prejudice, adhering to the ethical concept of trustworthiness. This approach was critical to maintaining the reliability and credibility of the study process. The reviewers' interpretations were open, ethical, and truthful, ensuring that the findings presented are both reliable and credible. Unlike other types of study, scoping research does not necessitate the acquisition of sensitive, confidential, or highly personal data from participants; as a result, many ethical guidelines that apply to other types of research do not apply to scoping reviews. The assessment, interpretation, and analysis of the chosen literature were reviewed and discussed, and conclusions were drawn. However, several methodological limitations of the included studies should be noted. Sample size variability refers to the relatively small sample sizes of the studies, which may limit the generalisability of their findings. Diagnostic criteria inconsistencies could potentially affect the consistency of diagnoses across studies. Geographical bias could also play a role, as the majority of the studies were conducted in Western countries, particularly the United States.
CONCLUSION
This review reveals that children and adolescents with ASD are significantly burdened by comorbid medical and psychiatric conditions, which evolve dynamically across psychosocial developmental stages. Through a thematic synthesis of 19 peer-reviewed studies, we identified recurring patterns in the presentation and severity of these comorbidities, most notably anxiety disorders, ADHD, epilepsy, sleep disturbances, and gastrointestinal challenges. Importantly, these conditions often interact with ASD symptoms in complex ways that vary by age, functional level, and sociocultural context.
Although valuable insights have been drawn from research conducted in Western countries, the global relevance of findings is constrained by a paucity of evidence from African regions. This imbalance may result in diagnostic blind spots, underreporting, or mismatches in care protocols. Notably, the few African studies included in our review reported disproportionately higher rates of intellectual disability and epilepsy among children with ASD. This pattern may reflect underlying contextual factors, such as limited diagnostic resources, late identification of ASD, or overlapping health burdens, which merit deeper investigation to clarify the influence of local health systems, sociocultural norms, and resource disparities.
To improve both diagnostic precision and care equity, future research must adopt longitudinal and context-sensitive approaches. This includes leveraging both qualitative insights and computational tools, such as data mining, predictive modelling, and AI-assisted phenotyping, to detect early markers of comorbid risk. Moreover, early intervention strategies tailored to developmental stages should be adapted for diverse populations, guided by cross-cultural validation studies.
By situating comorbidity research within a developmental and global health framework, our review advocates for interdisciplinary and culturally attuned practices that can respond to the evolving clinical realities of ASD.
IMPLICATIONS FOR CLINICAL PRACTICE AND FUTURE RESEARCH
The findings of this scoping review have significant implications for both clinical practice and future research in the field of ASD and its comorbidities. For clinical practice, our review highlights the need for comprehensive assessment protocols that consider the wide range of potential comorbidities across different developmental stages. Clinicians should be aware that comorbidities may manifest differently at various ages and tailor their diagnostic and treatment approaches accordingly.
Furthermore, the discrepancies observed between Western and African studies underscore the importance of culturally sensitive diagnostic tools and interventions. Clinicians working with diverse populations should be mindful of potential cultural variations in the presentation and prevalence of comorbidities.
For future research, our findings point to several key areas that warrant further investigation. Longitudinal studies that track the progression and evolution of comorbidities from infancy through adolescence are required to better understand the developmental trajectory of these conditions in individuals with ASD. More research is required on the medical comorbidities associated with ASD, particularly in Western contexts, as our review found a relative lack of focus in this area compared to psychiatric comorbidities. Cross-cultural studies that examine the impact of environmental, societal, and healthcare factors on the prevalence and manifestation of ASD-related comorbidities are crucial for developing a more comprehensive global understanding of ASD. Further investigation into the efficacy of early intervention strategies for managing comorbidities in infants and toddlers with ASD is needed, given the potential for improved long-term outcomes.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contributions to the paper as follows: W.T.: Study conception and design; C.M. and A.M.: Writing - original draft preparation. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ASD | = Autism Spectrum Disorder |
| ADHD | = Attention-Deficit/Hyperactivity Disorder |
| PROSPERO | = International Prospective Register of Systematic Reviews |
| OSF | = Open Science Framework |
| PDD-NOS | = Pervasive Developmental Disorder–Not Otherwise Specified |
| ODD | = Oppositional Defiant Disorder |
AVAILABILITY OF DATA AND MATERIALS
Authors may deposit their datasets openly to Zenodo Repository, in addition to their own or their institutional archives. For more details please visit https://openpsychologyjournal.com/
ACKNOWLEDGEMENTS
The authors extend their sincere thanks to Daniel Felix, whose research assistance was crucial in enriching this study’s depth and breadth.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.